2019 DRX9000® Study
Figure 1

Figure 2
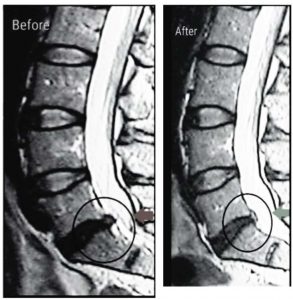
Figure 3
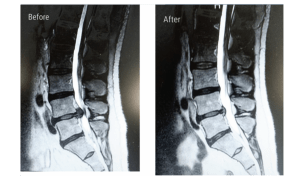
Figure 4
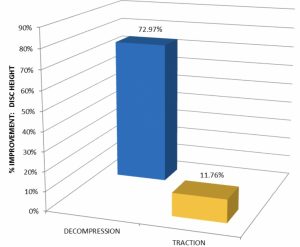
Figure 5
Ahmed R. El-Zayata , Wael Gomaha, Ahmed H. Aldesoukyb Departments of a Rheumatology, Physical Medicine and Rehabilitation, b Radiology, Faculty of Medicine, Al Azhar University, Cairo, Egypt Correspondence to Dr. Ahmed Ramzy El-Zayat, MD Rheumatology, Physical Medicine and Rehabilitation, Misr Algadyda, Triumph.
Spinal decompression therapy as an alternative modality for management of low back pain and radicular pain caused by lumbar disc herniation or protrusion
Abstract
Background
Recent studies have suggested that motorized nonsurgical spinal decompression AQ5 can reduce chronic low back pain (LBP) due to lumbar disc herniation or protrusion.
Aim
The purpose of this study was to evaluate the efficacy of motorized non-surgical spinal decompression by the DRX9000® device in the reduction of LBP and radicular pain caused by lumbar disc herniation or protrusion and whether it correlated with MRI changes in disc height or not.
Patients and methods
This study was carried out on 73 patients with chronic LBP attributed to disc protrusion selected from outpatients of rheumatology and rehabilitation clinics at Abdul Latif Jameel Hospital for Medical Rehabilitation, Jeddah, Saudi Arabia; these patients were divided into two groups. The first group comprised 39 patients who underwent a 6-week treatment protocol of motorized non-surgical spinal decompression via the DRX9000® , and the other group comprising 34 patients underwent a 6-week physiotherapy with deep heat modalities and ordinary traction; pain assessment using a visual analog scale with MRI was carried out before and after treatment. Paired t-test or linear regression was used, as appropriate, with P less than 0.05 considered to be statistically significant
Results
The main outcomes were a significant improvement in LBP in both groups using visual analog scale, but radicular pain and disc height using MRI were significantly improved in group 1 compared with group 2.
Conclusions
The study concluded that non-surgical spinal decompression was associated with a reduction in back pain and radicular pain and with an increase in disc height and can be used as an alternative modality for discogenic LBP.
Keywords:
decompression system, DRX9000® , lumbar disc prolapse, LBP
Figure 1

Figure 2
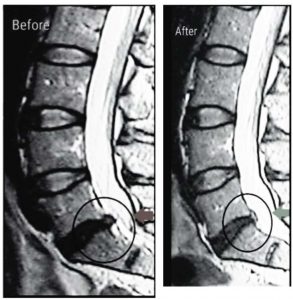
Figure 3
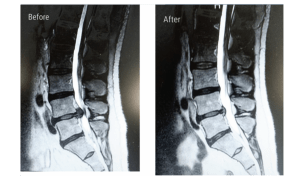
Figure 4
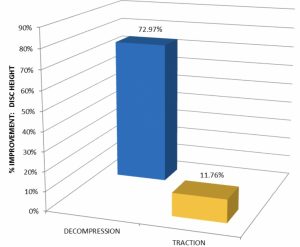
Figure 5
Ahmed R. El-Zayata , Wael Gomaha, Ahmed H. Aldesoukyb Departments of a Rheumatology, Physical Medicine and Rehabilitation, b Radiology, Faculty of Medicine, Al Azhar University, Cairo, Egypt Correspondence to Dr. Ahmed Ramzy El-Zayat, MD Rheumatology, Physical Medicine and Rehabilitation, Misr Algadyda, Triumph.
Introduction
More than 80% of the population will suffer from low back pain (LBP) at some point in their lives [1]. LBP is the main factor causing limiting activity in patients less than 45 years old, the second most frequent cause for doctor’s visits, and the third most common reason for surgical procedures [2]. LBP is of significant socioeconomic relevance, as it affects patients’ quality of life, may lead to a loss of productivity temporarily and enormous medical and indirect costs, or even permanent disability [3].
The two most common diseases causing chronic LBP are discogenic LBP, which is caused by disc degeneration, responsible for 39% of cases, and disc herniation, accounting for just less than 30% of cases of LBP. The clinical pathology of both discogenic LBP and disc herniation is related to the anatomical structure of the intervertebral disc [4].
The traditional management of LBP was nonsurgical treatment with analgesia supplemented by physiotherapy. There are many modalities of physiotherapy such as massage, spinal manipulation, exercises, acupuncture, back school, and cognitive behavioral therapy [4]. They also report some of the problems associated with simple traction, such as fatigue, triggering of muscle spasm, the patient’s inability to tolerate the force or position, and the exacerbation of pain [5].
Thus, the other treatment modality is motorized decompression, a technique designed to decrease
pressure on the discs, vertically expand the intervertebral space, and restore disc height [6]. Spinal decompression systems such as the DRX9000® have been launched into clinical practice in the last few years for the treatment of LBP. These systems provide a noninvasive intervention for the treatment of LBP of discogenic origin.
DRX9000® True Non-surgical Spinal Decompression System was FDA (the US Food and Drug Administration) approved; it applies spinal distraction forces by using a sensitive computerized feedback mechanism to provide relief of LBP and symptoms associated with herniated discs, bulging or protruding intervertebral discs, degenerative disc disease, posterior facet syndrome, and sciatica [7].
Richmond et al. [7] stated that the DRX9000® aims to relieve pain by enlarging intradiscal spaces, reducing herniation, and decreasing intradiscal pressure during treatment.
Aim
The goal of this study was to evaluate the efficacy of motorized non-surgical spinal decompression by the DRX9000® device in the reduction of LBP and radicular pain caused by lumbar disc herniation or protrusion and whether it correlated with MRI changes in disc height or not.
Patients and methods
This study was carried out on 73 patients; their ages ranged from 21 to 45 years; they had chronic LBP with radicular pain caused by disc protrusion or herniation, as diagnosed by MRI of the lumbosacral spine, and the duration of the disease was more than 12 weeks [8]. They were selected from outpatients attending the rehabilitation clinic in Abdul Latif Jameel Hospital for Medical Rehabilitation, Jeddah, Saudi Arabia, during the period spanning from January 2016 to September 2017; consent was taken from every patient for the treatment and to be included in this study. Patients with other causes of LBP, the presence of osteoporosis, vertebral fracture, displacement, weakness in the lower limbs, impaired sensation in both lower limbs or spondylolisthesis and pregnant women were excluded from the study. The patients were divided into two groups.
(1) First group: this group comprised a total of 39 patients, 23 (58.97%) male patients and 16 (41.03%) female patients; their ages varied between 21 and 43 years with a mean age of 32.06±7.09 years, and the duration of disease varied from 16 to 56 weeks, with a mean duration of 34.26±13.45 weeks. Their weights varied between 64 and 97 kg. This group underwent decompression using the DRX9000® .
(2) Second group: this group comprised a total of 34 patients, 19 (55.88%) male patients and 15 (44.22%) female patients; their ages varied between 23 and 45 years with a mean age of 33.21±7.23 years, and the duration of disease varied from 18 to 53 weeks, with a mean duration of 32.43±12.22 weeks. Their weight varied between 61 and 93 kg. This group underwent physiotherapy including deep heating modalities and ordinary traction.
All patients were subjected to full history taking; clinical examination including site of tenderness, straight leg raise (SLR) test, motor and sensory assessment, and range of motion of the lumbar spine were carried out before and after completion of sessions. Visual analog scale (VAS) from 0 to 10 was used before and after completion of the treatment course for assessment of LBP during a flexion-extension range of motion and for assessment of radicular pain in the lower limbs. Radiological assessment included radiographic lumbosacral spine anterioposterior and lateral view and MRI lumbosacral spine to support a diagnosis of chronic discogenic LBP due to bulging, protruding or herniated intervertebral discs that may have been brought on by degenerative disc disease. MRI was also repeated after completion of the
treatment course to assess whether there were changes in disc height or not.
MRI was performed before the start of treatment and after the end of treatment using a 3.0 T magnetic resonance unit (MAGNETOM Verio, A Tim System; Siemens, Erlangen, Germany). The patients were positioned in the supine position and scans were performed: (a) sagittal T1 images from T12 to the sacrum (repetition time: 670 ms; echo time: 12 ms, slice thickness: 4 mm), (b) sagittal T2 images from T12 to sacrum (repetition time: 3000–3600 ms; echo time: 87–114 ms, slice thickness: 4 mm), and (c) axial T2 images from L1 to S1 (repetition time: 3000–3600 ms; echo time: 87–114 ms, slice thickness: 4 mm).
Intervertebral disc height
Intervertebral disc height of the lumbar spine was measured on midsagittal MRI from the middle of the superior border of the disc to the middle of the inferior border of the discwith theinclusion of both end plates. In our study,we detect the difference of disc height between two MRIs to avoid personal variation in disc height. Paired t-test or linear regression was used, as appropriate, with P less than 0.05 considered to be statistically significant.
Treatment protocol
(1) First group: a total of 39 patients receivedtreatment with the DRX9000® (Axiom Worldwide, Tampa, Florida, USA) according tothe intervention’s operating guidelines [9].
(2) Second group: a total of 34 patients receivedphysiotherapy including ultrasound,transcutaneous electrical nerve stimulation(TENS), and vertebral traction.
The protocol of the DRX9000® includes 20 sessions of spinal decompression over a 6-week period with 30- min active treatment sessions. Each patient was administered treatment five times per week for the first 2 weeks and three times per week for a further 2 weeks, and it was then tapered down to two sessions per week for the last 2 weeks. At the start of the session, the patient is fitted into the supine position. To start active treatment, the machine pulls the patient gently on the lower harness while the upper harness remains stationary, thus distracting the patient’s spine. A safety button can be pushed at any time by the patient to release all tension immediately. The initial decompression force was adjusted to patient tolerance, starting at 4.54 kg (10 lbs) less than half their body weight. If a patient described the decompression pull as ‘strong or painful,‘ this distraction force was decreased by 10–25%. In subsequent treatment sessions, the distraction force was increased as tolerated to final levels of 4.54–9.07 kg (10–20 lbs) more than half their body weight. After the end of each therapy session, a cold pack with electrical muscle stimulation was applied to help paravertebral muscles consolidate after treatment.
RESULTS
First group
Before patients underwent the treatment sessions, the mean of LBP by VAS was 7.66±1.62, and, after sessions, it was 2.23±1.67 with P value less than 0.005 considered as significant difference. With regard to the lower extremity radicular pain assessed by VAS, before taking sessions, the mean was 7.43 ±2.50, and, after sessions, it was 1.33±1.79 with P value less than 0.005 considered as significant difference. There was one (2.56%) patient who presented with severe LBP after five sessions, and the patient stopped undergoing the sessions. There were six (15.38%) patients who had muscular pain during the sessions, but they continued the sessions; pain persisted in four of them (10.25%) until the end of the sessions.
MRI
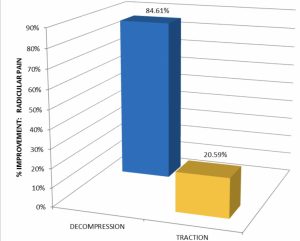
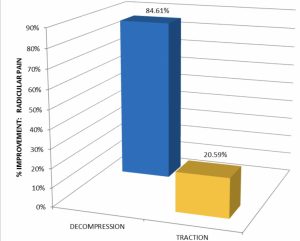
There were improvements of disc height in 27 (72.97%) patients, ranging from 1.1 up to 5.3 mm,with a mean of 2.31±1.24 mm. LBP was improved in 29 (74.36%) patients while radicular pain improved in 33 (84.61%) patients; disc height improved in 27 (72.97%) patients.
Second group
Before patients underwent the treatment sessions, the mean of LBP by VAS was 7.55±1.78, and, after sessions, it was 4.14±1.52, with P value less than 0.005 considered as significant difference. With regard to lower extremity radicular pain by VAS, before patients underwent the treatment sessions, the mean was 7.32±2.32, and, after sessions, it was 6.82±1.95 with no significant difference, P value greater than 0.005.
MRI
There were improvements of disc height in four (11.76%) patients, ranging from 0.1 up to 0.3 mm, with a mean of 0.043±0.091 mm. LBP was improved in 25 (73.53%) patients while radicular pain improved in seven (20.59%) patients; disc height improved in four (11.76%) patients. When we compared both groups, we found that there were nonsignificant differences in the improvement of LBP and a highly significant difference in the improvement of radicular pain and disc height between both groups (Figs 1–4 and Tables 1–4).
DISCUSSION
Discogenic pain is a major problem in the lumbar area, and it may be caused by progressive annular breakdown and tearing, which cause pain by stimulating pain fibers in the outer one-third of the annulus and by compression over the nerves’ roots. Spinal decompression systems using the DRX9000® have become a noninvasive intervention for the treatment of LBP caused by disc protrusion or herniation by expanding the intervertebral space and reducing the disc protrusion. Our study showed that there was an improvement in back pain and lower extremities’ radicular pain with the decompression system; the improvement was more significant in lower extremities’ pain than back pain.
Figure 1

There was a significant improvement in the disc heights of the majority of patients by the decompression system. Comparing with the control group, we found highly significant improvement in patients treated with the decompression system with regard to radicular pain and disc height compared with other physiotherapy modalities. Our study was in agreement with Richmond et al. [7] who stated that Non-surgical Spinal Decompression.
Figure 2
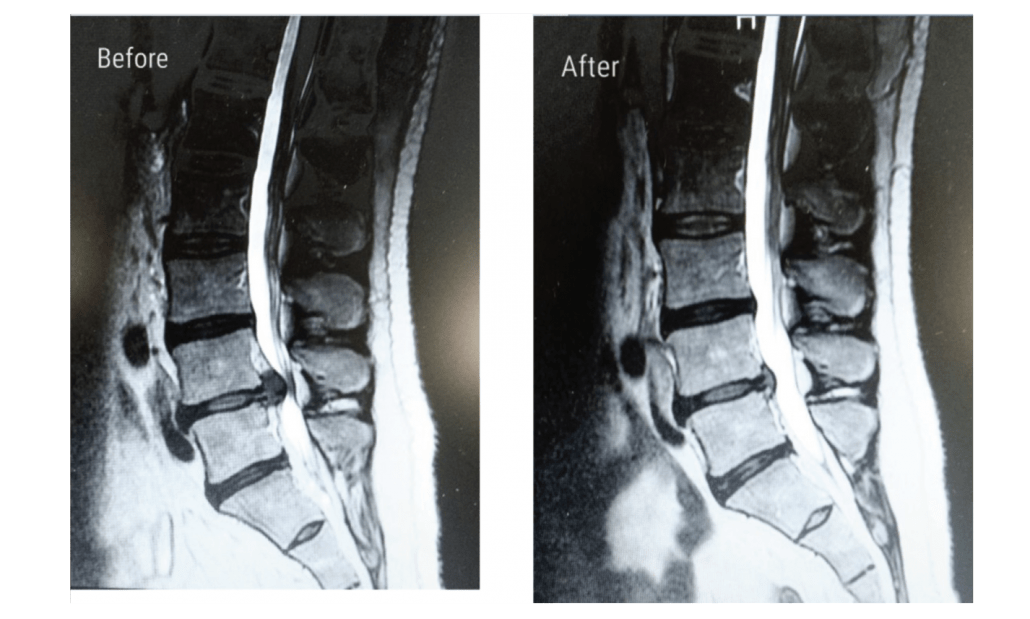
Figure 3
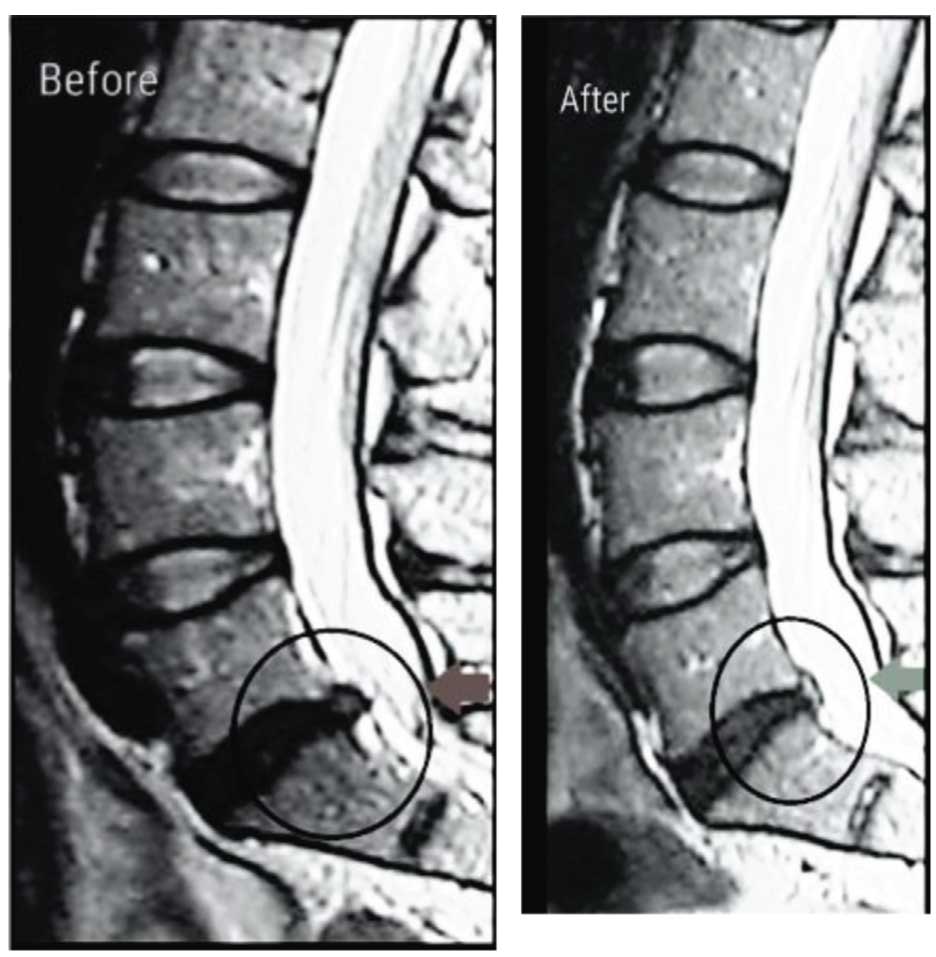
Figure 4
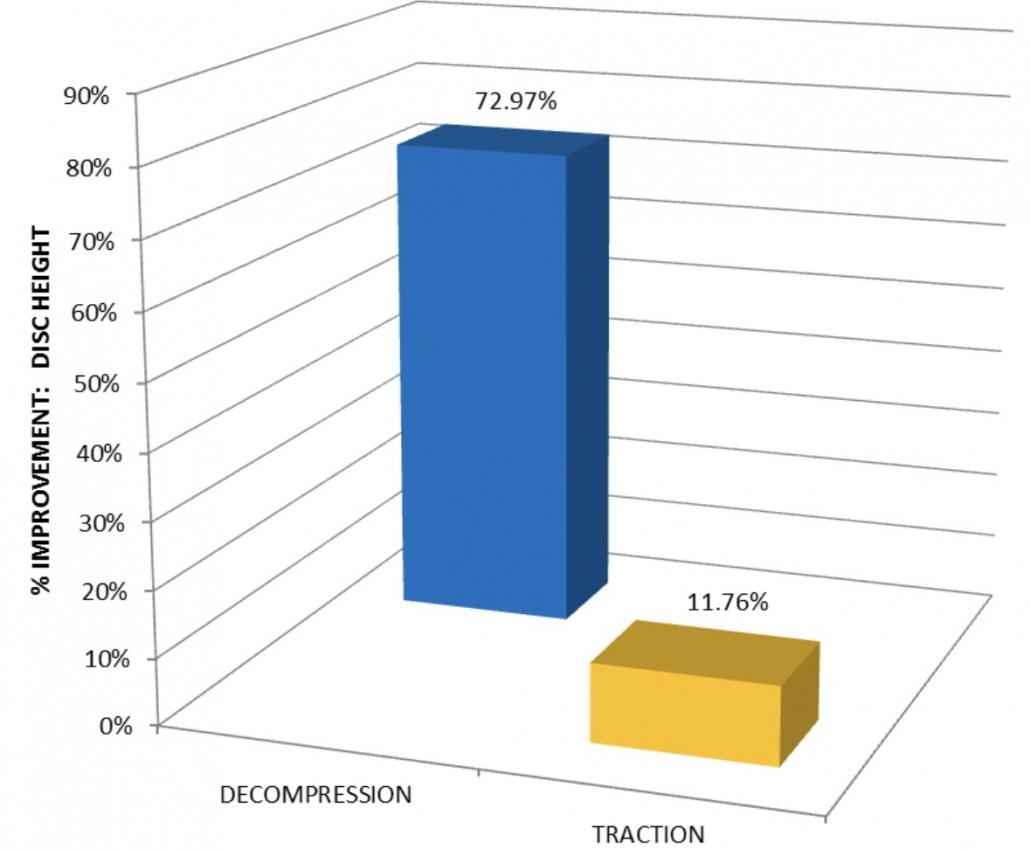
Figure 5
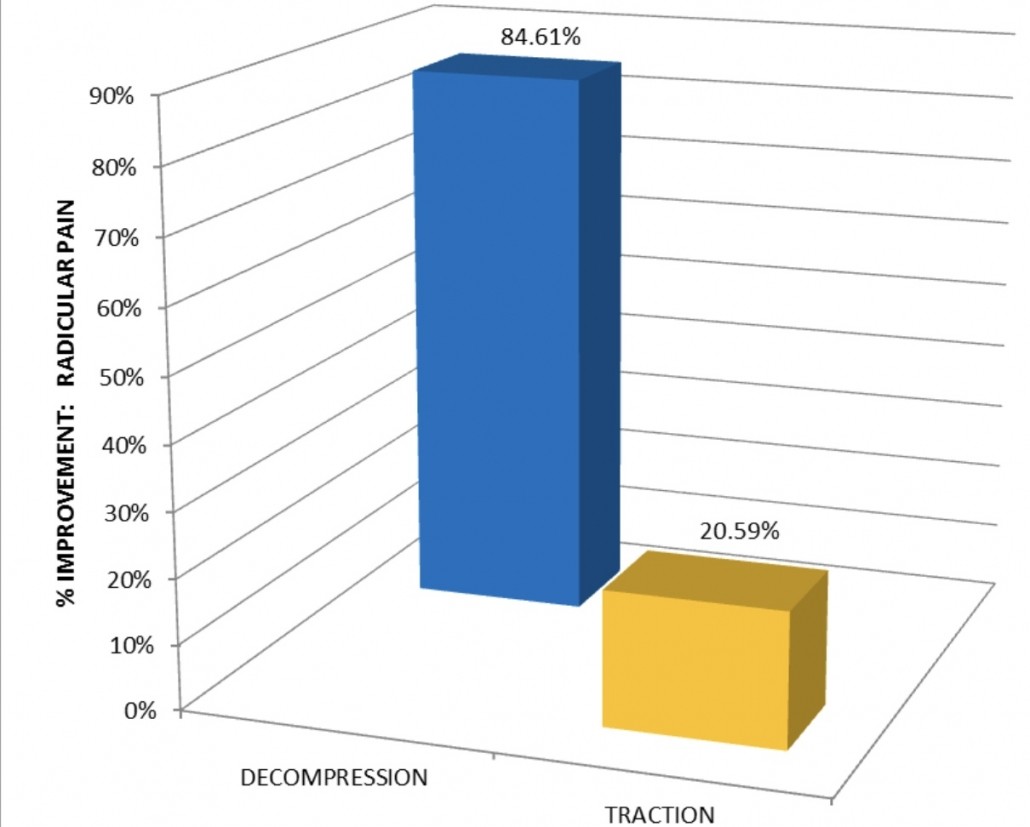
% Improvement : Radicular Pain
Table 1 Comparison between the two groups
| Group 1 | Group 2 | |
| LBP before treatment | 7.66±1.62 | 7.55±1.78 |
| LBP after treatment | 2.23±1.67 | 4.14±1.52 |
| LBP % of improvement | 74.36 | 73.53 |
| Radicular pain before treatment | 7.43±2.50 | 7.32±2.32 |
| Radicular pain after treatment | 1.33±1.79 | 7.32±2.32 |
| Radicular pain % of improvement | 84.61 | 20.59 |
| Improvement in disc height | 2.31±1.24 | 0.043±0.091 |
| % improvement in disc height | 72.97 | 11.76 |
| LBP, low back pain |
Table 2 Percentage of improvement between the two groups
| Group 1 (%) |
Group 2 (%) |
P value | |
| LBP % of improvement | 74.36 | 73.53 | less then 0.05 |
| Radicular pain % of improvement |
84.61 | 20.59 | less then 0.01 |
| % improvement in disc height | 72.97 | 11.76 | less then 0.01 |
System by using the DRX9000® resulted in relief of LBP and symptoms associated with herniated discs, bulging or protruding intervertebral discs, degenerative disc disease, posterior facet syndrome and sciatica by using a sensitive computerized feedback mechanism. In another study, Apfel et al. [10] found that spinal decompression by DRX9000® for treating chronic discogenic LBP caused relief of pain and restoration of disc height, and there was a correlation between pain reduction and degree of restoration of disc height, which agreed with our study; however, the difference between this study
Table 3 Percentage of improvement between the two groups
| Before | After | P value | |
| LBP | 7.66±1.62 | 2.23±1.67 | less then 0.05 |
| Radicular pain | 7.43±2.50 | 1.33±1.79 | less then 0.05 |
Table 4 Percentage of improvement between the two groups
| Before | After | P value | |
| LBP | 7.55±1.78 | 4.14±1.52 | less then 0.05 |
| Radicular pain | 7.32±2.32 | 7.32±2.32 | less then 0.05 |
and our study was that they assessed disc height by using CT scan but we used MRI. Thomas et al. [11] agreed with our study, as they stated that non-surgical spinal decompression (DRX9000®) had effective treatment of discogenic back pain by decompressive force, as pain was reduced in 86% of patients who were candidates for surgery, and mechanical function was restored in 92%, but 2% of patients presented with pain after 90 days and 3% of patients suffered a relapse.
Leslie et al. [9] also stated that, when patients are treated with DRX9000® completing the full 6-week course of spinal decompression, patients’ pain reduced and patient activity function became better, as measured by the Oswestry Disability Index. The decompression system is a good modality for treating discogenic LBP, as it reduces pain, improves function and decreases surgical intervention.
Conclusion
Overall, this study suggests that treatment with the DRX9000® non-surgical spinal decompression system, reduced patient’s chronic LBP and radicular lower extremities’ pain, with patients requiring fewer analgesics, compared with other modalities. Moreover, improvement in disc height measured by MRI has been found.
Financial support
and sponsorship Nil.
Conflicts of interest There are no conflicts of interest.
References
- Zhang Yg, Guo Tm, Guo X, Wu Sx. Clinical diagnosis for discogenic low back pain. Int J Biol Sci 2009; 5:647–658.
- Andersson GB. Epidemiological features of chronic low back pain. Lancet 1999; 354:581–585
- i style=”text-align: left;”>3 Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 2008; 8:8–20.
- Chou R, Huffman LH. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society American College of Physicians clinical practice guideline. Ann Intern Med 2007; 147:492–504.
- Macario A, Richmond C, Auster M, Pergolizzi JV. Treatment of 94 outpatients with chronic discogenic low back pain with the DRX9000® : a retrospective chart review. Pain Pract 2008; 8:11–17.
- Ramos G, Martin W. Effects of vertebral axial decompression on intradiscal pressure. J Neurosurg 1994; 81:350–353.
- Richmond C, Florio F, Wilhelm JM, Auster M. Magnetic resonance imaging findings after treatment with a non-surgical spinal decompression system (DRX9000TM) − case report. US Musculoskelet Rev 2007; 2007:50–52.
- Rozenberg S. Chronic low back pain: definition and treatment. Rev Prat 2008; 58:265–272.
- Leslie J, Pergolizzi JV, Macario A, Apfel CC, Clair D, Richmond C. Prospective evaluation of the efficacy of spinal decompression via the DRX9000® for chronic low back pain. J Med 2008; 9:2–8.
- Apfel CC, Cakmakkaya OS, Martin W, Richmondl C, Macario A, George E, et al. Restoration of disk height through non-surgical spinal decompression is associated with decreased discogenic low back pain: a retrospective cohort study. BMC Musculoskelet Disord 2010; 11:155.
- Thomas A, Gionis B, Eric Groteke DC. Spinal decompression. Orthop Technol Rev 2003; 5–6:36–39.
