DRX9000® Special Report Research
Nonsurgical Spinal DecompressionTo Treat Chronic Low Back Pain
INTRODUCTION
In most industrialized countries, chronic low back pain (LBP) is recognized as a widespread condition.1 Until recently, conventional wisdom held that most episodes of acute LBP are benign and self-limited, with 80% to 90% of attacks resolving in about 6 weeks and that 5% to 10% of patients who experience an episode of acute LBP go on to experience chronic back pain. This expectation is now in doubt: It is currently recognized that acute LBP tends to relapse, and many patients experience recurring episodes, leading to a chronic condition. Current evidence shows that 25% to 60% of patients will experience another episode of LBP at 1 year or longer after the initial episode.2
Most episodes of acute LBP are resolved without recourse to medical care. If a patient receives medical care, pain and disability usually resolve and the patient can return to work, typically within 1 month.3 However, in as many as 1 in 3 patients, chronic LBP eventually develops that persists indefinitely and is disabling. Patients can experience constant pain and become functionally impaired, with 1 in 5 reporting substantial limitations to their activities.3,4 In a literature review of 30 population studies of LBP published between 1966 and 1998, the prevalence of LBP ranged from 12% to 33%, 1-year prevalence from 22% to 65%, and lifetime prevalence from 11% to 84%. Approximately 25% of adults in the United States report having experienced LBP in the past 3 months, and the proportion of physician visits attributed to back pain has changed little since the 1990s.5
Economic and Social Burden Of Low Back Pain
In the United States, LBP is the second most common reason for a visit to a physician, the fifth most common cause of admission to a hospital, and the third most common indication for surgery.6 A minority of patients with back pain account for the majority of health care costs related to back pain, indicating that the potential cost of treating all patients with back pain is much higher than the actual cost.3,7 LBP is among the top 10 reasons for visits to internists and the most common and most expensive reason for work disability in the United States.8 It is also a frequent cause of early retirement for medical reasons.
Prevalence and Burden of Low Back Pain
A study of the national prevalence and correlates of low back and neck pain among adults in the United States found that in 2002, the 3-month prevalence of LBP was 34 million.9 The annual prevalence of chronic LBP is currently between 15% and 45%; the average age-related prevalence of persistent LBP is approximately 15% in children, adolescents, and adults and 27% in the elderly.2 In the United States, the financial and social costs of LBP include impaired function, limited activity, and a reduced quality of life, as well as disability, underemployment, reduced productivity, and direct medical costs. In the United States in 1998, direct health care costs attributable to LBP were estimated at $26.3 billion, and indirect costs related to days lost from work were substantial.3 Among US workers aged 40 to 65 years, exacerbations of back pain and lost productivity cost employers up to $7.4 billion per year; workers with chronic back pain accounted for 71.6% of this cost. Behind these statistics are many other workforce costs, such as the need for hiring and training replacement workers, the effect on co-workers’ productivity, and the loss of leisure time.2
In addition to the obvious discomfort, inconvenience, and societal costs of LBP, a recent cross-sectional study of the comorbid conditions related to back pain found that compared with a normal reference population, patients with LBP had significantly more neck pain, upper back pain, foot pain during exercise, headache, migraine, sleep problems, heat sensations, anxiety, and sadness or depression. This finding led the authors to conclude that patients with LBP experience what is effectively a “syndrome,” with an effect beyond that of the isolated spinal pain.10 Although research on back pain has focused primarily on younger, working adults, there is clear evidence that back pain is 1 of the most frequent complaints in older people and a proximate cause of functional limitations and perceived difficulty in performing the activities of daily living (ADLs). It is also a risk factor for future disability.2
Management of Low Back Pain
Diagnosing low back pain
There are wide variations in testing and diagnostic routines, in addition to a multitude of potential treatment approaches and professional uncertainly about the optimal approach to the management of LBP.11 More than 85% of patients who initially consult a primary care physician for back pain have nonspecific LBP, or pain that cannot easily be attributed to a specific disease or spinal abnormality. Efforts to identify specific anatomic sources of the pain in such patients are frequently unsuccessful.3
Intervertebral disks, facet joints, ligaments, fascia, muscles, and nerve root dura have all been identified as structures that can cause pain in the low back. Only abnormalities of the facet joints, intervertebral disks, and sacroiliac joints have been conclusively demonstrated to be causes of pain with the use of established diagnostic techniques. Central neural plasticity, changes in membrane excitability, and gene expression may all influence the perception of pain.12 Individual psychosocial characteristics such as job satisfaction may also affect the development of chronic LBP.13,14
For the purposes of screening and initial treatment, most patients can be classified into 2 categories: surgical and nonsurgical. The vast majority of patients should initially undergo conservative nonsurgical treatment. A focused history and physical examination will establish specific underlying conditions and can indicate the presence and level of neurologic involvement.3,15 Patients can then be subcategorized into 3 groups: a) those with nonspecific LBP; b) those with back pain potentially associated with radiculopathy or spinal stenosis (suggested by the presence of sciatica or pseudoclaudication); and c) those with back pain potentially associated with other spinal causes. These include the small number of patients with serious or progressive neurologic deficits or underlying conditions that require prompt evaluation (eg, tumor, infection, cauda equina syndrome), as well as conditions such as ankylosing spondylitis and vertebral compression fracture.
Mechanical low back or leg pain accounts for 97% of all cases of LBP. The term mechanical refers to an anatomic or functional abnormality without underlying malignant, neoplastic, or inflammatory disease. Lumbar strain or sprain will be the final diagnosis in 70% of these cases. Other mechanical and spinal phenomena that can help guide appropriate therapies include degenerative disk disease, a herniated disk, spinal stenosis, osteoporotic compression fracture, and spondylolisthesis. The incidence of the various causes of LBP may vary substantially according to the demographic characteristics and referral patterns in any specific clinical practice. For example, spinal stenosis and osteoporosis will be more common in geriatric practices.
Mechanical causes of LBP include injury to the lumbosacral muscles and ligaments, facet joint or sacroiliac joint arthropathy, and discogenic disease due to degenerative changes.16 In patients with back and leg pain, a history typical of sciatica indicates a herniated disk.17 More than 90% of symptomatic lumbar disk hernias occur at the L4-5 and L5-S1 levels. A focused examination that includes the straight leg raise test and a neurologic examination that includes an evaluation of the strength and reflexes of the knees, strength of the great toes, dorsiflexion of the feet, plantar flexion of the feet, ankle reflexes, and distribution of sensory symptoms should be conducted to assess the presence and severity of nerve root dysfunction.3
Discogenic pain most commonly affects the lower back, buttocks, and hips and is likely a result of internal disk degeneration. Disk degeneration is likely due to the injury and subsequent repair of the annulus fibrosus, where growth factors, macrophages, and mast cells involved in the repair of the injured annulus fibrosus contribute to subsequent deterioration. Discogenic pain may be due to progressive annular breakdown and tearing that stimulate pain fibers in the outer one-third of the annulus.18
Disk degeneration has been documented in asymptomatic groups of people ranging in age from 10 to 19 years, with 20% of people in their teens demonstrating mild disk degeneration.19 By 50 years of age, 10% of disks show degenerative pathology, and by 70 years of age, 60% of vertebral disks are severely degenerated. Disk degeneration alone is thought to be associated with sciatica, disk herniation and prolapse, alteration of disk height, adverse effects on spinal components such as muscles and ligaments, and potentially spinal stenosis.20
Current treatment options
Many alternatives are available for the evaluation and management of LBP, but little consensus has been established on which options are appropriate or preferable for various scenarios. The 3 major categories of treatment of LBP are surgical, nonsurgical, and pharmacologic. The appropriate treatment may depend on the origin and severity of the presenting condition.
When patients initially present with LBP and coexisting severe or progressive neurologic symptoms, computed tomography (CT) or magnetic resonance imaging (MRI) is indicated. Some symptoms will warrant a surgical consultation. The majority of episodes of LBP are mechanical or musculoskeletal in origin and respond well to exercise and conservative pharmacologic treatment with nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen. Nonsurgical, noninvasive therapies are the most frequently and appropriately prescribed.
Conservative treatments vary widely and are individualized to the patient. Acute LBP is usually treated through self-care with exercise, analgesics such as acetaminophen and NSAIDs or skeletal muscle relaxants, superficial heat therapy, and patient education. If the condition is unresponsive to conservative therapy, other options include more robust pharmacologic alternatives (muscle relaxants, systemic corticosteroids, and in rare cases opioids), spinal manipulation, acupuncture, acupressure, and more recently developed therapies such as transcutaneous electrical nerve stimulation (TENS).
Other noninvasive modalities for treating chronic LBP include exercise regimens such as Pilates and yoga, spinal decompression (manual, mechanized, and motorized), back schools, and cognitive-behavioral therapy (CBT).3 The effectiveness of the treatment often varies, as does the evaluation of treatment success. The utility of each modality can depend on the origin of the pain.21
Pain of discogenic origin may be the most intractable type of chronic LBP.22 Patients with severe LBP of discogenic origin that does not respond to conservative medical management have the options of surgical spinal fusion, minimally invasive intradiscal electrothermal therapy (IDET), and other surgeries specific to the particular diagnosis.23,24 The intent of many surgical procedures is to decrease pressure in the intervertebral spaces. Various conservative nonsurgical therapies have also been used to achieve decompression, beginning with simple traction, mechanical traction, and motorized spinal decompression. However, a recent meta-analysis found that very few randomized controlled trials (RCTs) evaluating traction reported positive effects on LBP, and increased pain and intervertebral pressure have been reported after its use.25
New options for the nonsurgical treatment of low back pain
More recently, a variety of mechanized and motorized spinal decompression systems have been developed that address some of the possible pitfalls of simple traction. The first of these was the VAX-D (vertebral axial decompression system; Vat-Tech Inc.). Several other devices have appeared since then, including the DRX9000™ (Axiom Worldwide; (Figure 1), which is a motorized spinal decompression device, and the Accu-Spina System (North American Medical Corporation).
Some of the newest developments in mechanized spinal decompression systems were presented at the 2007 annual clinical meeting of the American Academy of Pain Management (AAPM).26 Spinetronics presented its Antalgic-Trak device, CERT HealthSciences presented its SpineMED Decompression Table, and Axiom Worldwide reported new data and new directions for its DRX9000™
Conservative treatments for low back pain
According to the most recent literature-supported recommendations released by the American College of Physicians and the American Pain Society, nonpharmacologic therapies for chronic LBP include acupuncture, exercise therapy, massage therapy, Viniyoga-style yoga, CBT or progressive relaxation, spinal manipulation, and intensive interdisciplinary rehabilitation.3,27,28 Other treatments include back school, interferential therapy, low-level laser therapy, lumbar supports, short-wave diathermy, TENS, ultrasonography, acupressure, neuroreflexotherapy, spa therapy, and simple motorized and computer-controlled traction.3,22

In general, treatments should be individualized and based on an assessment of the patient’s symptoms and responses to interventions, the experience and training of the primary care clinician, and the availability of specialists with relevant expertise. Patient expectations of benefit from a treatment also seem to influence outcomes. Moderately effective therapies for chronic LBP include acupuncture,27 exercise therapy, massage therapy, Viniyoga-style yoga,28 herbal medicine,29 CBT or progressive spinal manipulation, and intensive interdisciplinary rehabilitation, although the level of supporting evidence for the different therapies varies from fair to good.22 In meta-regression analyses, exercise programs that incorporate individual tailoring, supervision, stretching, and strengthening are associated with the best outcomes.22 TENS has not been proven effective for chronic LBP, and acupressure, neuroreflexotherapy, and spa therapy have not been studied in the United States. There is insufficient evidence on interferential therapy, low-level laser therapy, short-wave diathermy, and ultrasonography, and evidence is inconsistent for back schools, although some trials have demonstrated small short-term benefits.22
With the exception of continuous or intermittent traction, which has not been shown to be effective in patients with sciatica, few trials have evaluated the effectiveness of treatments specifically in patients with radicular pain or symptoms of spinal stenosis. At present, there is insufficient evidence to recommend any specific treatment as first-line therapy.22 Some interventions, such as intensive interdisciplinary rehabilitation, may not be available in all settings, and costs for similarly effective interventions can vary substantially.
For LBP of discogenic origin, some evidence indicates that both simple and motorized traction can expand the intervertebral space and reduce disk protrusion and intradiscal pressure.21,30,31 However, systematic reviews of clinical trials of traction for LBP with or without sciatica have found that traction is probably not effective in relieving pain compared with placebo, sham, or other treatments.25,32
In general, traction can be delivered manually via the patient’s weight while the patient is placed through a suspension device, or by having the patient pull on bars at the head of a specially designed table while he or she lies on the table with the pelvis secured. These types of traction can be difficult to standardize because of fatigue on the part of both patient and therapist or the patient’s inability to tolerate the force or the position.33 Additionally, the pull force is linear and may elicit a proprioceptive response that triggers paravertebral muscle contraction, reducing the distractive effect. Spinal decompression systems have overcome these limitations of conventional traction. These include the DRX9000™, a nonsurgical spinal decompression system cleared by the FDA in 2003, the VAX-D, and the Accu-Spina System. Although some nonrandomized studies of motorized spinal decompression reported reduction of pain, a systematic review of relevant randomized trials suggested that the published data are too heterogeneous to determine whether nonsurgical spinal decompression provides greater benefit to individuals with LBP than do other treatments.34
Surgical Versus Nonsurgical Treatment
Chronic LBP of discogenic origin may often be unrelieved by conservative management. Some patients with such pain turn to open surgical spinal fusion.22 Surgical treatments for disk prolapse are open discectomy, microdiscectomy, chemonucleolysis, automated percutaneous discectomy, laser discectomy, nucleoplasty, mechanical disk decompression, and manual percutaneous lumbar discectomy. For LBP that is related primarily to internal disk disruption, management includes total disk excision, IDET, and radio-frequency posterior annuloplasty. A number of fusion procedures are available for the treatment of degenerative disk disease. The success of all these surgical procedures, both minimally invasive and otherwise, is variable and has been found to be no better than that of nonintervention.2,23,2
The risks and inconveniences of surgery are such that some guidelines suggest a minimum of 3 months to 2 years of failed nonsurgical interventions before patients with nonspecific LBP are referred to possible surgery or other invasive interventions.3 Since the 1990s, the rates of low back fusions for patients with chronic LBP have increased rapidly, especially among patients older than 60 years of age. The increase in surgery has not been associated with a similarly rapid increase in efficacy for the procedure.35 The recent SPORT (Spine Patient Outcomes Research Trial) evaluated the efficacy of surgery in treating lumbar intervertebral disk herniation and lumbar degenerative spondylolisthesis.36,37 In a randomized clinical trial that compared standard open discectomy with individualized conservative management, including physical therapy, epidural steroid injections, NSAIDs, and opioids, the investigators found that surgery and conservative management were roughly equal in effectiveness for treating lumbar disk herniation.36
In a systematic review of randomized trials comparing the efficacy of surgical with that of nonsurgical care for discogenic LBP, the authors found that surgical care (for the most part lumbar fusion surgery) was slightly more efficacious than unstructured physical therapy. Highly structured rehabilitation with a CBT component appeared roughly equivalent to surgery in efficacy, with fewer complications. Interestingly, none of the studies in the review showed treatment-related differences in average back-specific disability outcome that met the FDA threshold for a clinically meaningful difference.24
The Newest Noninvasive Therapies
Noninvasive decompression is 1 modality that has attempted to address the need for nonsurgical interventions that specifically approach LBP of discogenic origin. Experimental data exist to support the concept that nonsurgical decompression reduces intradiscal pressure. This in turn may facilitate oxygen and nutrient uptake and improve disk metabolism and restoration. Types of traction in use today include motorized, mechanical, manual (in which the therapist exerts traction by using the patient’s arms and/or legs), auto, gravity-dependent (or inverted suspension), pneumatic, continuous, intermittent, bed rest, and underwater traction.25
The most recent Cochrane Review on the use of traction for LBP with or without sciatica included RCTs that examined any type of traction for the treatment of acute, subacute, or chronic nonspecific LBP without sciatica symptoms. The study reviewed the mechanical, manual (unspecific or segmental traction), auto, underwater, bed rest, continuous, and intermittent types of traction. (The authors did not distinguish between spinal decompression traction and the other forms of applied traction for their analyses.)
The review provided strong evidence that short- and longterm outcomes do not differ between continuous or intermittent traction and placebo, sham, or other treatments for patients with a mixed duration of LBP with or without sciatica.25 A randomized study that compared traction in a semi-reclined position at a 30-degree angle with physical therapy versus physical therapy alone found little difference between the 2 modalities, leading the authors to conclude that traction has no effect beyond that of the normal physical therapy regimen.32
There are few data to suggest that any major adverse events occur from the use of the various forms of traction available on the market as long as patients are screened correctly. In an overview of the adverse effects of traction, approximately 25% of studies reported some adverse effects, such as increased pain in 31% of the static traction group and 15% of the intermittent traction group, with the others reporting no adverse events.25
The DRX9000™ applies nonsurgical spinal decompression by using a sensitive computerized feedback mechanism. The DRX9000™ uses a split-table design to reduce friction between the patient and the device. The patient lies supine, and a chest and shoulder support system controls the upper body, with a knee rest to eliminate pelvic rotation. The apparatus has built-in air bladders, disk-angle pull adjustments, and harnesses, and it can increase the decompression force more slowly in the latter part of the therapy. The DRX9000™ spinal decompression device uses a motor pulley to deliver mechanized segmental distraction that can be delivered in a static or oscillatory fashion for a preselected duration; the location of lumbar spinal disease determines the best pullangle settings
The Current State of Research On Spinal Decompression
Basic Science
Certain traction techniques can cause an increase in intradiscal pressure, an event that is particularly detrimental in treating LBP associated with herniated disks and a neurocompressive etiology. Nonsurgical spinal decompression, a specialized form of powered traction, is available in several devices. Initial investigations were first focused on measuring intradiscal pressure in patients who had been treated with axial decompression before undergoing discectomy.22 In the study, the effect of the axial decompression system on pressure in the nucleus pulposus was measured before a scheduled discectomy in 5 patients with lumbar disk herniation confirmed by MRI by inserting a cannula into the nucleus pulposus of the L4-5 intervertebral disk and then connecting it to pressure monitors.
Distraction tension applied by the device reduced the intradiscal pressure to a negative level of as much as –100 to –160 mm Hg, with an inverse relationship between distraction tension and intradiscal pressure. Notably, the change in intradiscal pressure appeared to be minimal until a threshold distraction of 40 to 50 lb of tension had been achieved. When this threshold was exceeded, the intradiscal pressure decreased dramatically below the positive pressure observed before the application of decompressive tension.
Another group of investigators demonstrated that axial decompression was capable of improving dermatomal somatosensory evoked potentials (DSSEPs), presumably through decompressing the lumbar nerve root.38 Seven consecutive patients with a diagnosis of LBP and unilateral or bilateral L5 or S1 radiculopathy were studied bilaterally with DSSEPs before and after axial decompression therapy. MRI or CT was used to document disk herniation in all patients. After treatment, all patients had at least a 50% reduction in radicular symptoms and LBP, with 3 experiencing complete resolution of all symptoms. The average pain reduction was 77%.

Another investigation compared axial decompression treatment with TENS treatment in 44 patients with chronic LBP of longer than 3 months’ duration. The TENS treatments demonstrated a success rate of 0%, whereas axial decompression demonstrated a success rate of 68.4% (P < 0.001). A statistically significant reduction in pain and functional outcome was observed in the patients treated with axial decompression, but not in those treated with TENS.39
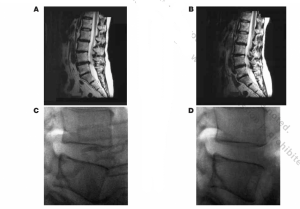
The evolution of technology has led to changes in force application, patient positioning, and the addition of passive restraint systems in the newer nonsurgical spinal decompression devices such as the DRX9000™. Investigators have reported early success with the DRX9000™ system based on objective radiologic observations of intervertebral disk height or measured bulging. In a small series of case studies, a group of investigators added new data to the hypothesis that such decompressive systems can, over time, increase disk volume and reduce herniation, as shown in the MRI findings of a patient (Figures 2A and 2B) and lateral radiograph of an asymptomatic healthy volunteer (Figures 2C and 2D).
A review of recent studies examined the efficacy of traction systems that include forms of motorized traction. A systematic literature review of motorized spinal decompression for the treatment of chronic discogenic LBP found 7 RCTs of motorized spinal decompression applied with various apparatus, including a split tabletop, a plain tabletop, and a friction-free couch with weights. Because only 3 of the 7 RCTs provided a description of the randomization procedure, none had blinded assessments of outcome, and the patient groups were heterogeneous.
For these reasons, the authors concluded that a qualitative review was more appropriate than a meta-analysis. Of the 7 RCTs, 6 reported no difference with motorized spinal decompression, and 1 reported reduced pain but not reduced disability. The lack of RCTs led the authors to also include 3 nonrandomized case series studies of motorized spinal decompression; the studies had no control groups. These studies each reported a 77% to 86% reduction in pain.34
The authors of the review concluded that the efficacy of spinal decompression with motorized spinal decompression for chronic discogenic LBP has not yet been conclusively demonstrated through standard trials. They suggested that this could be the result of heterogeneous patient groups and the difficulty of properly blinding researchers and patients to the modality being used. More rigorous studies with better randomization, control groups, and standardized outcome measures are needed to overcome the limitations of past studies.
Studies of New Decompression Systems
Several new devices use computer-controlled motorized spinal decompression to treat LBP, including the DRX9000™, the Antalgic-Trak, and the SpineMED Decompression Table. Currently, no clinical outcome data are available for the Antalgic-Trak and SpineMED systems, nor has any recent literature shown success with the older systems, such as the VAX-D.
A review of the published evidence regarding spinal decompression systems suggests that the data are inconclusive as to efficacy and that the studies are not adequate to permit validated conclusions. This problem of realistically assessing the efficacy of noninvasive, nonsurgical decompressive systems is being addressed, and future studies will provide the data needed to help physicians determine clinical treatment routines based on outcomes that demonstrate efficacy.
A mansucript in press reports data from a recent retrospective study of 94 outpatients with discogenic LBP lasting for more than 12 weeks. The review demonstrated decreased symptoms following DRX9000™ spinal decompression therapy.40 The patients were randomly selected from 4 clinics, and patients underwent motorized spinal decompression with the DRX9000™ for 8 weeks (mean). Each received 28- to 30-minute sessions daily for 2 weeks, tapering to 1 session per week. The treatment protocol also included lumbar stretching, the application of myofascial release or heat before stretching, and the application of ice and/or muscle stimulation afterward. The primary outcome measure was change in intensity of pain on a verbal numeric rating scale (NRS) ranging from 0 to 10 between baseline and the end of the treatment.
Of the enrolled patients, 63% were female and 95% were white. The mean age of the patients was 55 years. Of the subjects, 52% were employed and 41% were retired. Herniated disk was diagnosed in 73% of the cases and degenerative disk in 68%. Of the patients, 27% had both herniated and degenerative disks
The initial mean NRS score of 6.05 (standard deviation [SD], 2.3) at presentation decreased significantly to 0.89 (SD, 1.15; P < 0.0001) after completion of DRX9000™ treatment protocol. Analgesic use also decreased, and ADLs improved. At followup, patients reported a mean rate of LBP reduction of 90% (SD,1.15), and a satisfaction score of 8.55 on a scale ranging from 0 to 10 (median, 9).40
This study was retrospective and lacked a control or comparison group, and the 4 clinics differed in their use of adjunctive modalities. Nonetheless, such positive clinical outcomes from the initial review of patients treated with the DRX9000™ warranted further investigation in a more rigorous prospective clinical study with an expanded patient population presenting with chronic LBP.
A pilot study was completed and presented at the 2007 annual meeting of the AAPM.26 The study was a prospective, multicenter, nonrandomized Phase II clinical trial to evaluate the effectiveness and safety of the Axiom Worldwide DRX9000™ for the active treatment of chronic LBP with a standardized clinical research multimodal protocol. Eighteen patients with chronic LBP for more than 3 months underwent a series of 20 DRX treatments (28 minutes each) for 6 weeks in which 5 sessions in the first 2 weeks were tapered to 1 session the last week. The multimodal treatment protocol included ice after the DRX sessions, lumbar stretching exercises, and adjunct analgesics as required. Assessments of pain, analgesic use, functionality, satisfaction, ADLs, and safety were collected through examinations, questionnaires, and patient diaries. The average daily LBP score fell from 6.4 to 3.1 (P < 0.01) after 2 weeks of treatment and was reduced to 0.8 (scale 0-10) after the completion of all treatments at 6 weeks (P < 0.001). In addition to significant reduction in LBP, the patients noted an improvement in function as measured by a decrease in the average Oswestry Disability Index score from 23.7 to 5.5 at the end of therapy.
In this pilot study, the DRX9000™ showed promise in treating chronic LBP arising from multiple causes. Although it is unlikely that improvements of this magnitude are a placebo effect in patients with chronic LBP lasting on average 526 weeks and with failed multiple previous therapeutic interventions, a larger DRX9000™ trial with 1-year patient follow-up is under way, and a randomized blinded or sham-treatment study is scheduled to follow the larger trial. Additional longerterm outcome data must also be collected from DRX9000™- treated patients to determine the long-term benefits, and comparative outcome trials need to be performed to document the potential value of the DRX9000™ nonsurgical spinal decompression system in the routine treatment of chronic LBP. The efficacy of the DRX9000™, in both the short and long term, needs to be compared with that of other therapies currently in widespread clinical use by using a set of standardized and validated multiple outcome variables, as were used in the pilot study.
An abstract presented at the 2006 World Congress of the International Society of Physical and Rehabilitation Medicine in Seoul, South Korea, reported results from a recent study that compared the efficacy of spinal decompression with the DRX3000 (the international version of the DRX9000™) with that of traction in treating lumbosacral disk herniation.41 In the study, 65% of patients treated with the DRX3000 achieved a decrease of more than 50% in their Visual Analogue Scale (VAS) pain score, 25% achieved a decrease of more than 80%, and 10% a decrease of more than 30%. These results were in contrast to those of the patients treated with conventional traction, 60% of whom achieved at least a 30% decrease in their VAS score and 30% of whom achieved no decrease or a decline in pain of less than 30%. The DRX9000™ has been studied extensively outside the United States (Table).
| Trial Name | Country | No. of Patients | Prospective? (Yes or No) | Main Results |
| The Effect of Spinal Decompression Therapy Compared With Conventional Traction in Lumbosacral Disk Herniation41 | Korea | 35 | Y | Mean reduction in VAS score for conventional traction (n=15) was 1.93±0.83; mean VAS score reduction with spinal decompression therapy (n=20) was 4.35±2.21a |
| Nonsurgical Spinal Decompression: Treatment of Low Back Pain by Spinal Decompression and Spinal Exercises42 | India | 75 | Y | Spinal decompression with DRX9000™ plus heat/cold packs and physical therapyb |
| Efficacy of Spinal Decompression Combined With Transforaminal Steroid Injection Versus Transforaminal Steroid Injection in Patient With Lumbar Disk Herniation43 | Korea | 41 | Y | TFI plus spinal decompression with DRX9000™ |
| Effects of Spinal Decompression (DRX9000™) for Lumbar Disk Herniation44 | Japan | 7 | Y | Spinal decompression with DRX9000™ plus physical therapyb |
| True Nonsurgical Spinal Decompression Therapy™45 | Korea | 84 | Y | Spinal decompression with DRX3000 plus cold and interferential therapyb |
| Clinical Studies for Spinal Decompression System DRX9000™46 | Russia | 21 | DRX9000™ plus heat/cold packs and physical therapyb |
Future Directions
There is a clear need for well-designed prospective randomized long-term controlled trials to compare the efficacy of spinal decompression with that of other treatments for discogenic chronic LBP. Investigation of the mechanism of action of the DRX9000™ will continue through the use of MRI and positron emission tomography to measure differences in disk spaces before and after intervention. The basic treatment parameters must also be refined to determine the ideal angle, force required, and duration and frequency of treatments. The more individualized and precise these parameters become, the better they may be prescribed for each patient. A multiple-arm, matrix-design study is currently being planned that will test these variables
Conclusion
In modern times, chronic LBP is a widespread and debilitating phenomenon. The causes and experiences of LBP are as varied as the patients who live with it, and no 1 treatment is comprehensively effective. Discogenic pain can be particularly difficult to treat. The most current evidence-based guidelines recommend conservative treatment for at least 2 months, and often much longer, before a surgical option is considered. Surgery is associated with risks, and the outcome in many patients with discogenic back pain is unpredictable. A nonsurgical, noninvasive treatment is a potentially viable option for treating intractable discogenic pain. The DRX9000™ computerized nonsurgical spinal decompression systems were designed to provide maximum patient benefits with the use of a noninvasive approach that may help minimize health care resources and offer a potentially optimal therapeutic approach to the treatment of LBP. Well-designed long-term trials are being conducted to further validate its use.
References
- Maetzel A, Li L. The economic burden of low back pain: a review of studies published between 1996 and 2001. Best Pract Res Clin Rheumatol. 2002;16(1):23-30.
- Boswell MV, Trescot AM, Datta S, et al. Interventional techniques: evidencebased practice guidelines in the management of chronic spinal pain. Pain Physician. 2007;10(1):7-111.
- Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7): 478-491.
- Diamond S, Borenstein D. Chronic low back pain in a working-age adult. Best Pract Res Clin Rheumatol. 2006;20(4):707-727.
- Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from US national surveys, 2002. Spine. 2006;31(23):2724-2727
- Krishnaney AA, Park J, Benzel EC. Surgical management of neck and low back pain. Neurol Clin. 2007;25(2):507–522.
- Engel CC, von Korff M, Katon WJ. Back pain in primary care: predictors of high health-care costs. Pain. 1996;65(2-3):197-204.
- Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002;137(7):586-597
- Strine TW, Hootman JM. US national prevalence and correlates of low back and neck pain among adults. Arthritis Rheum. 2007;57(4):656-665.
- Hagen EM, Svensen E, Eriksen HR, et al. Comorbid subjective health complaints in low back pain. Spine. 2006;31(13):1491-1495
- . Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344(5): 363-370
- Coderre TJ, Katz J, Vaccarino AL, Melzack R. Contribution of central neuroplasticity to pathological pain: review of clinical and experimental evidence. Pain. 1993;52(3):259-285
- Carragee EJ, Alamin TF, Miller JL, Carragee JM. Discographic, MRI and psychosocial determinants of low back pain disability and remission: a prospective study in subjects with benign persistent back pain. Spine J. 2005;5(1):24-35.
- Borenstein DG. Epidemiology, etiology, diagnostic evaluation, and treatment of low back pain. Curr Opin Rheumatol. 1999:11(2):151-157.
- McCamey K, Evans P. Low back pain. Prim Care. 2007;3(1)4:71-82
- Peng B, Hao J, Hou S, et al. Possible pathogenesis of painful intervertebral disc degeneration. Spine. 2006;31(5):560-566.
- Vroomen PC, de Krom MC, Knottnerus JA. Diagnostic value of history and physical examination in patients suspected of sciatica due to disc herniation: a systematic review. J Neurol. 1999;246(10):899-906.
- Anderson MW. Lumbar discography: an update. Semin Roentgenol. 2004;39(1):52-67.
- Miller JA, Schmatz C, Schultz AB. Lumbar disc degeneration: correlation with age, sex, and spine level in 600 autopsy specimens. Spine.1998;13:
173-178. - Atlas SU, Nardin RA. Evaluation and treatment of low back pain: an evidencebased approach to clinical care. Muscle Nerve. 2003;27:265-284.
- Ramos G, Martin W. Effects of vertebral axial decompression on intradiscal pressure. J Neurosurg. 1994;81(3):350-353.
- Chou R, Qaseem A, Snow V, et al. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147(7):492-504.
- Andersson GBJ, Mekhail NA, Block JE. Treatment of intractable discogenic low back pain. A systematic review of spinal fusion and intradiscal electrothermal therapy (IDET). Pain Physician. 2006;9(3):237-248.
- Mirza SK, Deyo RA. Systematic review of randomized trials comparing lumbar fusion surgery to nonoperative care for treatment of chronic back pain. Spine. 2007;32(7):816-823.
- Clarke JA, van Tulder MW, Blomberg SE, et al. Traction for low-back pain with or without sciatica. Cochrane Database Syst Rev. 2007;(2):CD003010
- Leslie J, Richmond C, Macario A, et al. Pilot: Effectiveness and safety of nonsurgical spinal decompression. Paper presented at: 18th Annual Meeting of the American Academy of Pain Management; September 27-30, 2007; Las Vegas, NV.. Manheimer E, White A, Berman B, et al. Meta-analysis: acupuncture for low back pain. Ann Intern Med. 2005;142(8):651-663.
- . Manheimer E, White A, Berman B, et al. Meta-analysis: acupuncture for low back pain. Ann Intern Med. 2005;142(8):651-663.
- Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing yoga, exercise, and a self-care book for chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2005;143(12):849-856.
- Gagnier JJ, van Tulder MW, Berman B, et al. Herbal medicine for low back pain: a Cochrane review. Spine. 2007;32(1):82-92.
- Gupta RC, Ramarao SV. Epidurography in reduction of lumbar disc prolapse by traction. Arch Phys Med Rehabil. 1978;59(7):322-327
- Onel D, Tuzlaci M, Sari H, Demir K. Computed tomographic investigation of the effect of traction on lumbar disc herniations. Spine. 1989;14(1):82-90.
- Borman P, Keskin D, Bodur H. The efficacy of lumbar traction in patients with low back pain. Rheumatol Int. 2003;23(2):82-86.
- Tekeoglu I, Adak B, Bozkurt M, et al. Distraction of lumbar vertebrae in gravitational traction. Spine. 1998;23(9):1061-1063.
- Macario A, Pergolizzi JV. Systematic literature review of spinal decompression via motorized traction for chronic discogenic low back pain. Pain Pract. 2006;6(3);171-178.
- Deyo RA, Gray DT, Kreuter W, et al. United States trends in lumbar fusion surgery for degenerative conditions. Spine. 2005;30(12):1441-1445
- Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296(20):2451-2459.
- Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med. 2007;356(22):2257-2270.
- Naguszewski WK, Naguszewski RK, Gose EE. Dermatomal somatosensory evoked potential demonstration of nerve root decompression after VAX-D therapy. Neurol Res. 2001;23(7):706-714.
- Sherry E, Kitchener P, Smart R. A prospective randomized controlled study of VAX-D and TENS for the treatment of chronic low back pain. Neurol Res. 2001;23(7):780-784.
- Macario, A, Richmond, C, Auster, M, et al. Treatment of 94 outpatients with chronic discogenic low back pain with the DRX9000®: a retrospective chart review. Pain Practice (in press).
- Kim H-S, Kim D-H, Huh K-Y. The effect of spinal decompression therapy compared with conventional traction in lumbosacral disc herniation. Program and abstracts of the 4th World Congress of the International Society of Physical and Rehabilitation Medicine; June 10-14, 2007; Seoul, South Korea. Abstract OP04-5.
- Hiranandani M. Nonsurgical spinal decompression: treatment of low back pain by spinal decompression and spinal exercises. Program and abstracts of the 45th Annual Indian Association of Physiotherapists Conference; February 2-4, 2007; Kolkata, India.
- Lee SH. Efficacy of Spinal Decompression Combined with Transforaminal Steroid Injection versus Transforaminal Steriod Injection in Patient with Lumbar Disc Herniation. Society of Rehabilitation; submitted 2007.
- Naoyuki O, Itabashi A, Kusano S, et al. Effects of Spinal Decompression DRX9000™) for lumbar disc herniation. Journal of Saitama Kenou Rehabilitation. 2006;6:38-42.
- Park JK. Nonsurgical spinal decompression therapy. Axiom Worldwide Abstract.
- Minukov GN, Vorobiev EV. Clinical studies for spinal decompression system: DRX9000™. Conducted in the Neurology Unit of Municipal Clinical Hospital; Moscow, Russia. May 13-July 24, 2006.