DRX9000® Pain Practice Research 2008
Treatment of 94 Outpatients With
Chronic Discogenic Low Back
Pain with the DRX9000®:
A Retrospective Chart Review
Alex Macario, MD, MBA*; Charlotte Richmond, PhD†; Martin Auster, MD, MBA‡; Joseph V. Pergolizzi, MD§
*Departments of Anesthesia and Health Research & Policy, Stanford University School of Medicine, Stanford, California; † Biomedical Research & Education Foundation, LLC, Miami Beach, Florida; ‡ Department of Radiology, Johns Hopkins University School of Medicine, Baltimore, Maryland, § Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland, U.S.A.
Abstract
Background: This study’s goal was a retrospective chart audit of 100 outpatients with discogenic low back pain (LBP) lasting more than 12 weeks treated with a 2-month course of motorized spinal decompression via the DRX9000® (Axiom Worldwide, Tampa, FL, U.S.A.).
Methods: Patients at a convenience sample of four clinics received 30-minute DRX9000® sessions daily for the first 2 weeks tapering to 1 session/week. Treatment protocol included lumbar stretching, myofascial release, or heat prior to treatment, with ice and/or muscle stimulation afterwards. Primary outcome was verbal numerical pain intensity rating (NRS) 0 to 10 before and after the 8-week treatment.
Results: Of the 100 initial subjects, three withdrew their protected health information, and three were excluded because their LBP duration was less than 12 weeks. The remaining 94 subjects (63% female, 95% white, age = 55 (SD 16) year, 52% employed, 41% retired, LBP median duration of 260 weeks) had diagnoses of herniated disc (73% of patients), degenerative disc disease (68%), or both (27%). Mean NRS equaled 6.05 (SD 2.3) at presentation and decreased significantly to 0.89 (SD 1.15) at end of 8-week treatment (P < 0.0001). Analgesic use also appeared to decrease (charts with data = 20) and Activities of Daily Living improved (charts with data = 38). Follow-up (mean 31 weeks) on 29/94 patients reported mean 83% LBP improvement, NRS of 1.7 (SD 1.15), and satisfaction of 8.55/10 (median 9). Conclusions: This retrospective chart audit provides preliminary data that chronic LBP may improve with DRX9000® spinal decompression. Randomized double-blind trials are needed to measure the efficacy of such systems.
Key Words: chronic pain, low back, disc disease, mechanical, spinal decompression
Address correspondence and reprint requests to: Alex Macario MD, MBA, Professor of Anesthesia and Health Research & Policy, Department of Anesthesia H3580, Stanford University School of Medicine, Stanford, CA 94305-5640, U.S.A. Tel: +1 650 498 6810; E-mail: [email protected]. Reprints will not be available from authors. Submitted: July 10, 2007; Revision accepted: October 1, 2007
INTRODUCTION
Chronic low back pain is an expensive benign condition in industrialized countries.1 In a literature review of 30 population studies of low back pain between 1966 and 1998, the prevalence of low back pain at any given moment ranged from 12% to 33%, 1-year prevalence ranged from 22% to 65%, and lifetime prevalence ranged from 11% to 84%.2 Mechanical causes may be either injury to lumbosacral muscles and ligaments, facet joint or sacroiliac joint arthropathy, or discogenic disease due to degenerative changes. Discogenic pain most commonly affects the lower back, buttocks, and hips and is thought to be related to injury and subsequent repair of the anulus fibrosus.3 Treatments vary widely, and should be individualized to the patient. If noninvasive modalities are preferred, many options exist such as oral analgesics,4 muscle relaxants,5 exercises,6 acupuncture,7 manipulation,8 or back school.9
Although data exist supporting the use of traction to widen the intervertebral space,10 reduce disc protrusion11 and intradiscal pressure,12 and improve motor evoked potentials13 and leg mobility,14 systematic reviews of clinical trials of traction for low back pain with or without sciatica have found that traction is probably not effective in improving pain, compared to placebo, sham or other treatments.15–20
In general, traction can be delivered manually by the therapist via the weight of the patient through a suspension device,21 or by the patient pulling the bars at the head of the table while lying on a specially designed table with the pelvis secured.22 These types of traction can be difficult to standardize because of the patient’s as well as the therapist’s fatigue, or intolerance by the patient to the force or position.23,24 Additionally, the pull force is linear and may elicit the body’s proprioceptive response that triggers paravertebral muscle contraction, which may reduce the distractive effect.
Several axial decompression systems have been developed to overcome these drawbacks. These systems include the DRX9000® (Axiom Worldwide, Tampa, FL, U.S.A., approved by FDA in 2003), the VAX-D (VatTech, Inc., Palm Harbor, FL, U.S.A., approved by the FDA in 1996), and the Accu-Spina System (North American Medical Corporation, Aventura, FL, U.S.A., approved by FDA in 2000). Although some nonrandomized studies of motorized spinal decompression reported pain reduction,25–28 a systematic review of relevant randomized trials suggests that published data are too limited to determine whether vertebral axial decompression provides benefit to individuals with low back pain (over other nonsurgical treatments).29
The goal of this study was to perform a retrospective chart audit to assess outcomes of a sample of outpatients with discogenic low back pain of more than 12 weeks treated with a 2-month course of motorized spinal decompression via the DRX9000®.
METHODS
This study was granted exempt status by a central institutional review board (Quorum Review) prior to study initiation. A partial waiver of the Health Insurance Portability and Accountability Act (HIPAA) was received following approval of the telephone screening instrument. Protected health information reviewed during this study was accessed in a manner to ensure the privacy and confidentiality of patient health information in accordance with the Privacy Rule of the HIPAA, Title 45, U.S. Code of Federal Regulations 164.501, 164.508, and 164.512.
This study was a retrospective review of 100 charts of adults cared for at four clinics (a convenience sample), one hospital-based and three free-standing, in Ohio and Illinois. A prospective power analysis indicated that 100 patients would be sufficient to demonstrate a 2-point reduction in the verbal numerical pain intensity rating (0 to 10, an 11-point scale), with baseline pain score of 6 and a standard deviation of 3, at a level of significance of P = 0.05 and power of 95%. Investigators have reported that a minimum of 20-mm difference on a written, self-reported visual analog scale is required to indicate a clinically important difference in chronic low back pain.30
When the investigator (C.R.) arrived at the clinic to examine the charts, the office assistant was asked to randomly select charts of patients. Inclusion criteria were patients more than 18 years old receiving a full course of treatment with DRX9000®, with one of the following diagnoses: herniated disc, bulging or protruding intervertebral discs, degenerative disc disease, posterior facet syndrome, and sciatica.
Patients with the following conditions were not eligible for spinal decompression treatment: pregnancy, prior lumbar fusion, cancer metastasis, severe osteoporosis, spondylolisthesis (unstable), spine compression fracture, aortic aneurysm, pelvic or abdominal cancer, disc space infection, severe peripheral neuropathy, hemiplegia, paraplegia, or cognitive dysfunction. Worker’s compensation patients were excluded from our study.
The sample size at each clinic was created as the number of charts that could be reviewed in 1 day, with an overall total of 100.
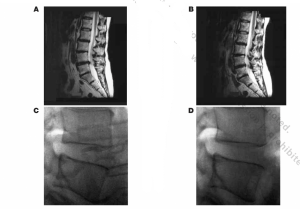
A single investigator (C.R.) reviewed these medical records (patients greater than 18 years of age with discogenic low back pain lasting more than 12 weeks) by using a standardized data collection form, available from the investigators upon request. Criteria for discogenic pain diagnosis included appropriate history and physical exam findings, supported by magnetic resonance imaging (MRI) findings.
For the DRX9000®, a split table design is used to reduce friction on the lumbar muscles. With the patient lying supine, a chest and shoulder harness controls the upper body. A knee rest eliminates pelvic rotation. The DRX9000® apparatus has built-in air bladders, disc angle pull adjustments, harnesses, and can increase the distraction force more slowly in the latter part of the decompression
Treatment protocol was individualized to the characteristics of the patient. The DRX9000® employs a motor pulley to deliver mechanized segmental distraction that can be delivered in a static or oscillatory fashion for a preselected duration. For example, the location of lumbar spine level disease (from the MRI) determines pull angle settings to target the affected lumbar disc. The typical pull angle setting was 18 degrees (range 6 to 30). Initial weight was set as 50% of patient’s weight minus 10 lb. (Table 1)
Treatment was delivered for 28 to 30 minutes daily for the first 2 weeks, three times per week for two more weeks, tapering to one session the last week for an average of 8 weeks. The weight was raised in increments of 5 to 10 lb per session for the first three sessions as tolerated until a final weight of 50% body weight plus 10 to 20 lb was reached. Treatment protocol included instruction on lumbar stretching exercises, myofascial release or heat prior to DRX9000® treatment, with cold packs and/or muscle stimulation after DRX9000® sessions.
Outcome measures including a verbal numerical pain intensity rating (0 to 10, an 11-point scale), analgesic use, and activities of daily living were assessed before the first DRX9000® session and after the last DRX9000® session. Data abstracted from the medical record depended on what each clinic recorded in the chart. Patients were phoned a minimum of 4 weeks after their last treatment to obtain longer-term follow-up. If after three attempts the patient was unreachable, we mailed a written survey questionnaire to get follow-up data. At this follow-up, we asked, “How satisfied were you with the DRX9000® treatment (0–10 scale)? 0 = Not satisfied 10 = Very satisfied)” and “What percent improvement in your low back pain did the DRX9000® provide?”
Of the 100 initial subjects, three patients withdrew their protected health information, and three patients initially studied were excluded from the final analysis because their back pain was less than 12 weeks in duration. Data on these three patients were inadvertently collected (even though they did not meet inclusion criteria), but this was not discovered until the database was analyzed.
Table 2 has details on the final sample size of 94. Not enough patients were enrolled to determine if the clinic was an independent predictor of outcome.
Table 1. Spinal Decompression Parameters Used for Treatment
- Initial weights (lb)
- Final weights (lb)
- Mean
- 57
- 74
- Low
- 17
- 20
- High
- 100
- 145
Statistics
Descriptive statistics are provided. Inferential statistics (Wilcoxon signed-rank test for nonparametric data) were only performed for verbal numerical pain intensity rating (0 to 10), as this was the primary endpoint, as recorded in the office chart prior to initiating treatment and at the end of the 2-month treatment course.
RESULTS
Patient (Table 3), clinical (Table 4), and MRI characteristics (Table 5) of the 94 patients studied are summarized.
The pain reference patterns included nonspecific low back pain in 89% of patients; pain radiation into the buttock in 23% of patients; pain radiation into the thigh or lower leg, in 62% of patients. Finally, leg pain was more severe than back pain in 8% of patients and 13% of patients had previous spine surgery.
Table 2. Patients Studied at Each Site and Characteristics of Clinics
- Number of patients studied
- Total number of patients seen by clinic/year
- Annual DRX9000® case volume
- Year DRX9000® installed
- Clinic R
- 33
- 850
- 212
- 2003
- Clinic O
- 10
- 6500
- 300
- 2002
- Clinic M
- 20
- 1000
- 800
- 2004
- Clinic S
- 31
- New clinic
- New clinic
- 2005
Patients studied had received other treatments for their low back pain prior to initiating spinal decompression including chiropractic manipulation (64% of patients), physical therapy (45%), epidural steroids (35%), massage (21%), and acupuncture (14%).
The median pain duration was 260 weeks (mean 535 weeks, range 12 to 3120 weeks).
At time of initial presentation to the clinic prior to DRX9000® treatment, subjects reported a mean verbal numerical pain intensity rating equal to 6.05 (SD 2.3, range 2 to 10, median 6, 25th to 75th percentile 4 to 8) on 0 to 10 scale. This decreased to 0.89 (SD 1.15, range 0 to 5, median 0.5, 25th to 75th percentile 0 to 1) after the last DRX9000® spinal decompression session (P < 0.0001).
Analgesic use and activities of daily living improved by the end of the 8-week treatment regimen. (Tables 6 and 7)
No adverse events were noted.
Patients paid median out-of-pocket of $10 per session (mean $27).
Table 3. Demographics of Cohort
- Mean age (years)ci
- Mean height (inches)
- Mean weight (kg)
- Mean BM
- % female
- % white
- % African American
- % Hispanic
- % Asian
- Employment status
- % employed
- % retired
- 55 (SD 16)
- 68 (SD 4
- 90 (SD 20)
- 30 (SD 7)
- 63
- 95
- 2
- 2
- 1
- 52
- 41
- 6
Table 4. Clinical Characteristics of Patients
- Primary Diagnosis
- Herniated disc
- Degenerative disc disease
- Herniated disc and degenerative disc disease
- Sciatica
- %
- 73
- 68
- 27
- 12
Table 5. MRI Findings
- Disc most involved (%)
- T12-L1
- L1-L2
- L2-L3
- L3-L4
- L4-L5
- L5-S1
- Mean number of levels with degenerative changes 2.4
Disc findings (%) - Degenerative changes
- Bulge
- Protrusion
- Extrusion
- Other findings (%)
- Neural foramen compromise
- Nerve root compression/impingement
- Central stenosis 15
- Facet arthropathy
- Endplate changes 5
- Disc space narrowing
- Disc most involved (%)
- 2
- 1
- 8
- 39
- 36
- 2.4
- Mean number of levels with degenerative changes 2.4
Disc findings (%) - 28
- 37
- 29
- 5
- Other findings (%)
- 23
- 9
- 15
- 16
- 5
- 14
Table 6. Analgesic Use
- Analgesics
- Charts with data
- No medication (%)
- NSAIDs (%)
- Opioids (%)
- Steroids (%)
- Muscle relaxants (%)
- Gabapentin (%)
- At time of Initial Presentation
- n = 94*
- 43
- 39
- 24
- 3
- 13
- 3
- After Last Treatment
- n = 20
- 75
- 15
- 10
- 5
- 5
- 0
Table 7. Activities of Daily Living
-
Back Pain Interfered
with ADL - Charts with data
- Bathing (%)
- Dressing (%)
- Transferring (%)
- Walking (%)
- Sitting (%)
- Standing (%)
- Sleep (%)
- Other (%)
-
At Time of Initial
Presentation - n = 85
- 23
- 23
- 0
- 52
- 50
- 53
- 21
- 61
-
After Last DRX
Treatment - n = 38
- 0
- 0
- 0
- 1
- 2
- 3
- 0
- 2
Follow-Up
Of the 94 eligible subjects, 25 were reached by telephone. The others did not return a phone message or the contact phone number was incorrect. Questionnaires were mailed to these remaining patients, and seven questionnaires were received back in the mail (three of the patients withdrew their consents for use of protected health information). Thus, we analyzed data on 29 of the 94 patients (mean follow-up of 31 weeks, median 17 weeks).
At this follow-up, patients reported: a mean 83% (median 90%, range 0% to 100%) improvement in back pain, a mean low back pain score of 1.7 (median 1, range 0 to 6) and satisfaction with the DRX9000® treatment equal to a mean of 8.55 (median 9, range 5 to 10) on a 0 to 10 scale (0 = Not satisfied 10 = Very satisfied). None of these patients reported requiring procedural therapies (eg, surgery).
DISCUSSION
Retrospective studies such as this one can provide useful information by evaluating treatment patterns and outcomes in routine clinical practice, in a diverse patient population. Subjects in our study were mostly female, white, age in their fifties, with 52% being employed and 41% retired. Overall, our findings suggest that the use of spinal decompression administered via the DRX9000® apparatus may help reduce chronic low back pain. The study cohort had a mean verbal numerical pain score of 6.05 on 0 to 10 scale at time of initial presentation, which is consistent with low back pain scores in published studies.31 Pain scores decreased significantly to 0.89 at the end of 8 weeks of DRX9000® treatment.
We did not have control groups, making it difficult to know how much of the benefit was due to the spinal decompression itself or placebo or spontaneous recovery as the natural course of chronic discogenic pain includes periods of improvement of functional capacity and pain scores. In fact, the favorable natural history of low back pain has been hypothesized to be a reason for the proliferation of “unproved” treatments that may seem to be effective.32 No untoward complications were noted in the 94 patients studied that received spinal decompression via the DRX9000®.
Discogenic pain is a major problem in lumbar degenerative disc disease, and may be due to progressive annular breakdown and tearing which stimulates pain fibers in the outer one-third of the annulus.33 Experimental data exist to support the concept that spinal decompression reduces intradiscal pressure. This in turn may facilitate oxygen and nutrient uptake and improve disc metabolism and restoration.34,35
However, oftentimes the anatomic cause of persistent low back pain remains unknown. This is because structural imaging and symptoms are poorly correlated.36–38 Central nervous system neuroplasticity related to neuronal hyperactivity, changes in membrane excitability, and expression of new genes may perpetuate the perception of pain.39 Also, patients’ baseline psychosocial variables may affect the development of chronic low back pain.40 Job satisfaction, for example, remains a strong predictive factor for the identification of patients with acute low back pain who will develop chronic low back pain.41 Certainly, a multidisciplinary approach can help patients with chronic discogenic low back pain by providing cognitive-behavioral therapy, patient education, nonsteroidal anti-inflammatory drugs, and physical therapy.
Limitations
Assessment for low back pain usually includes four specific domains: pain intensity, back pain specific disability, patient satisfaction with treatment outcome, and a work disability assessment.42 We attempted to evaluate all four domains, but the incomplete data available in the chart review did not allow us to make complete assessments on all four domains. Analgesic use appeared to decrease (charts with data = 20 out of 94 subjects) and activities of daily living improved (charts with data = 38 out of 94 subjects). As this was a retrospective study, and we recorded what was performed for each patient, the lack of control for either the analgesic use or the use during the time off traction treatment could have influenced the results.
Also, the study was retrospective with variability in how the various clinics used adjunctive modalities such as lumbar stretching exercises, myofascial release or heat prior to treatment, and cold packs and/or muscle stimulation in posttreatment sessions. The telephone/ mail follow-up was performed to enhance the retrospective chart audit. It is not known if the patients in the nonresponder group improved, remained stable, or deteriorated.
Future Studies
The study was limited to established patients with chronic low back pain. Nonetheless, positive clinical outcomes from this initial review of patients treated with the DRX9000® is encouraging and warrants further investigation in a more rigorous prospective clinical study. Such studies are under way and have an expanded patient population with tighter control of the treatment protocol (and use of adjunct therapies such as ice, heat, massage, anti-inflammatory drugs, Transcutaneous Electrical Nerve Stimulator). Spinal decompression systems available commercially may have differences in design, such as position of patient (supine or prone), angle of pull (and whether it is adjustable), type of motor, use of feedback from tension sensors during distraction to attempt to minimize proprioceptive paravertebral reflex muscle contraction,43 and measurement of delivered forces. These may lead to differing physical responses to therapy, so studies of one type of apparatus should not readily be applied across all machines.
Before a final assessment can be made on the efficacy and safety (eg, number of complications) of motorized spinal decompression, investigations are needed to determine which patient types do well, and which patients do not do well, and how benefits persist with time. For example, our mean longer term follow-up of 31 weeks, for 29 of the 94 patients, revealed a continued mean 83% improvement in low back pain, with a mean pain score of 1.7. Future studies will need to determine how much of the positive health outcome can be attributed to a device-specific mechanism of action vs. a multidisciplinary treatment approach, the optimal amount of distractive tension (the “pull weight” [pounds] relative to the patient’s weight), whether patient positioning during spinal decompression affects outcome, the optimal angle of distraction, length of the pull and relaxation cycles, and frequency and duration of decompression sessions. As spinal decompression is a noninvasive modality, the benefits may not have to be as large to the patient as for other more invasive treatments.
Conclusions
Overall, this preliminary analysis suggests that treatment with the DRX9000® nonsurgical spinal decompression system reduced patient’s chronic low back pain with patients requiring fewer analgesics, and achieving better function. However, without control groups, it is difficult to know how much of the benefit was placebo, spontaneous recovery, or the treatment itself. Randomized double-blind trials are needed to measure the efficacy of such systems.
ACKNOWLEDGMENTS
This study was funded in part by Axiom Worldwide, 9423 Corporate Lake Drive, Tampa, FL 33634. Axiom did not participate in the data collection, analysis, or interpretation of the results contained in the article.
REFERENCES
- Maetzel A, Li L. The economic burden of low back pain: a review of studies published between 1996 and 2001. Best Pract Res Clin Rheumatol. 2002;16:23–30.
- Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord. 2000;13:205–217.
- Peng B, Hao J, Hou S, et al. Possible pathogenesis of painful intervertebral disc degeneration. Spine. 2006;31:560– 566.
- Hale ME, Dvergsten C, Gimbel J. Efficacy and safety of oxymorphone extended release in chronic low back pain. Results of a randomized, double-blind, placebo- and activecontrolled phase III study. J Pain. 2005;6:21–28.
- Shen FH, Samartzis D, Andersson GB. Nonsurgical management of acute and chronic low back pain. J Am Acad Orthop Surg. 2006;14:477–487.
- Long A, Donelson R, Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine. 2004;29:2593–2602.
- Leibing E, Leonhardt U, Koster G, et al. Acupuncture treatment of chronic low-back pain—a randomized, blinded, placebo-controlled trial with 9-month follow-up. Pain. 2002;96:189–196.
- Gay RE, Bronfort G, Evans RL. Distraction manipulation of the lumbar spine: a review of the literature. J Manipulative Physiol Ther. 2005;28:266–273.
- van der Roer N, van Tulder MW, Barendse JM, et al. Cost-effectiveness of an intensive group training protocol compared to physiotherapy guideline care for sub-acute and chronic low back pain: design of a randomised controlled trial with an economic evaluation. BMC Musculoskelet Disord. 2004;5:45.
- Gupta RC, Ramarao SV. Epidurography in reduction of lumbar disc prolapse by traction. Arch Phys Med Rehabil. 1978;59:322–327.
- Onel D, Tuzlaci M, Sari H, Demir K. Computed
tomographic investigation of the effect of traction on lumbar
disc herniations. Spine. 1989;14:82–90. - Ramos G, Martin W. Effects of vertebral axial decompression on intradiscal pressure. J Neurosurg. 1994; 81:350–353.
- Guechev G, Guechev A. Fast dynamics of voluntary muscle strength and motor evoked potentials after traction therapy in patient with lumbosacral root lesion. Electromyogr Clin Neurophysiol. 1996;36:195–197.
- Meszaros TF, Olson R, Kulig K, Creighton D, Czarnecki E. Effect of 10%, 30%, and 60% body weight traction on the straight leg raise test of symptomatic patients with low back pain. J Orthop Sports Phys Ther. 2000;30:595–601.
- Scheer SJ, Radack KL, O’Brien DR Jr. Randomized controlled trials in industrial low back pain relating to return to work. Part 2. Discogenic low back pain. Arch Phys Med Rehabil. 1996;77:1189–1197.
- Koes BW, Bouter LM, van der Heijden GJ. Methodological quality of randomized clinical trials on treatment efficacy in low back pain. Spine. 1995;20:228–235.
- van der Heijdan GJ, Beurskens AJ, Koes BW, Assendelft WJ, de Vet HC, Bouter LM. The efficacy of traction for back and neck pain: a systematic, blinded review of randomised clinical trial methods. Phys Ther. 1995;75:93–104.
- Harte AA, Baxter GD, Gracey JH. The efficacy of traction for back pain: a systematic review of randomized controlled trials. Arch Phys Med Rehabil. 2003;84:1542– 1553.
- Clarke J, van Tulder M, Blomberg S, de Vet H, van der Heijden G, Bronfort G. Traction for low back pain with or without sciatica: an updated systematic review within the framework of the Cochrane collaboration. Spine. 2006;31: 1591–1599.
- Clarke JA, van Tulder MW, Blomberg SE, de Vet HC, van der Heijden GJ, Bronfort G. Traction for low-back pain with or without sciatica. Cochrane Database Syst Rev. 2005;(4):CD003010.
- Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B. Changes in sagittal lumbar configuration with a new method of extension traction: nonrandomized clinical controlled trial. Arch Phys Med Rehabil. 2002;83:1585–1591.
- Tesio L, Merlo A. Autotraction versus passive traction: an open controlled study in lumbar disc herniation. Arch Phys Med Rehabil. 1993;74:871–876.
- Waddell G, McIntosh A, Hutchinson A, Feder G, Lewis M. Low back pain evidence review. London: Royal Coll General Practitioners; 1999
- Tekeoglu I, Adak B, Bozkurt M, Gurbuzoglu N. Distraction of lumbar vertebrae in gravitational traction. Spine. 1998;23:1061–1063.
- Gionis TA, Groteke E. Spinal Decompression. Orthopedic Technology Rev. 2003;5:36–39.
- Gose EE, Naguszewski WK, Naguszewski RK. Vertebral axial decompression therapy for pain associated with herniated or degenerated discs or facet syndrome: an outcome study. Neurol Res. 1998;20:186–190.
- Shealy CN, Koladia N, Wesemann M. Long-term effect analysis of IDD therapy in low back pian: a retrospective clinical pilot study. Am J Pain Manage. 2005;15:93–97.
- Naguszewski WK, Naguszewski RK, Gose EE. Dermatomal somatosensory evoked potential demonstration of nerve root decompression after VAX-D therapy. Neurol Res. 2001;23:706–714.
- Macario A, Pergolizzi J. Systematic literature review of spinal decompression via motorized traction for chronic discogenic low back pain. Pain Prac. 2006;6:171–180.
- Hagg O, Fritzell P, Nordwall A, Swedish Lumbar Spine Study Group. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12:12–20.
- Hurwitz EL, Morgenstern H, Kominski GF, Yu F, Chiang LM. A randomized trial of chiropractic and medical care for patients with low back pain: eighteen-month follow-up outcomes from the UCLA low back pain study. Spine. 2006;31:611–621.
- Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344:363–370.
- Anderson MW. Lumbar discography: an update. Semin Roentgenol. 2004;39:52–67.
- Matsui Y, Maeda M, Nakagami W, Iwata H. The involvement of matrix metalloproteinases and inflammation in lumbar disc herniation. Spine. 1998;23:863–868.
- Fujita K, Nakagawa T, Hirabayashi K, Nagai Y. Neutral proteinases in human intervertebral disc. Role in degeneration and probable origin. Spine. 1993;18:1766–1773.
- Weishaupt D, Zanetti M, Hodler J, Boos N. MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology. 1998;209:661–666.
- Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69–73.
- Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects: a prospective investigation. J Bone Joint Surg Am. 1990;72:403–408.
- Coderre TJ, Katz J, Vaccarino AL, Melzack R. Contribution of central neuroplasticity to pathological pain: review of clinical and experimental evidence. Pain. 1993;52: 259–285.
- Carragee EJ, Alamin TF, Miller JL, Carragee JM. Discographic, MRI and psychosocial determinants of low back pain disability and remission: a prospective study in subjects with benign persistent back pain. Spine J. 2005;5:24–35.
- Borenstein DG. Epidemiology, etiology, diagnostic evaluation, and treatment of low back pain. Curr Opin Rheumatol. 1999;11:151–157.
- Grotle M, Brox JI, Vollastad NK. Functional status and disability questionnaires: what do they assess? A systematic review of back-specific outcome questionnaires. Spine. 2005;30:130–140.
- Andersson GB, Schultz AB, Nachemson AL. Intervertebral disc pressures during traction. Scand J Rehabil Med Suppl. 1983;9:88–91.