Clinical and Imaging Outcomes of Non-Surgical Spinal Decompression for Lumbar Intervertebral Disc Lesions
Study by the University of South Florida | Journal of Contemporary Chiropractic | Vol. 8, Issue 1, 2025 | March 07, 2025 CDT
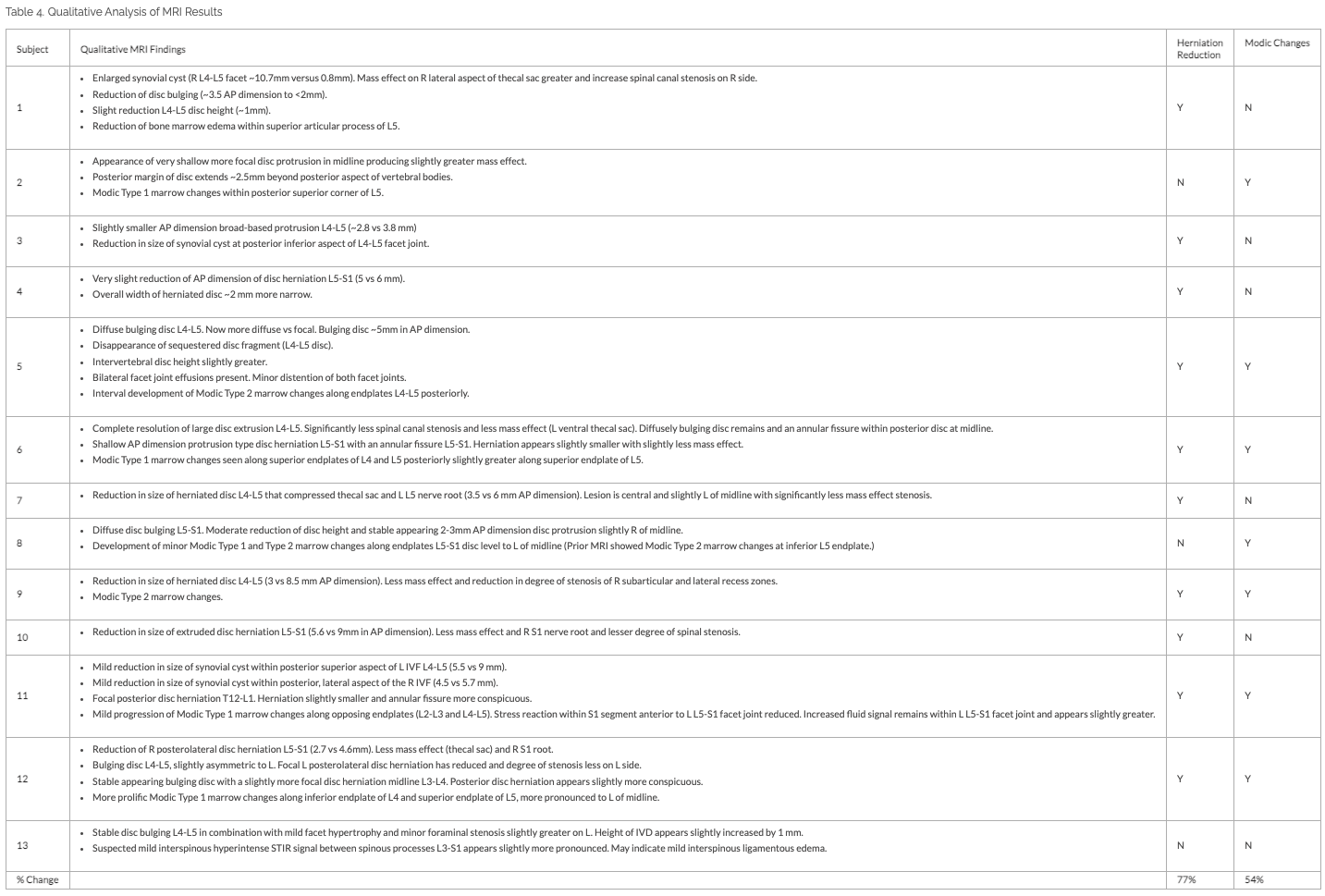
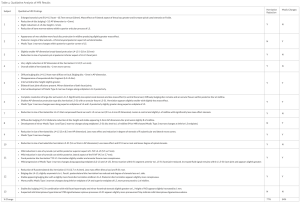
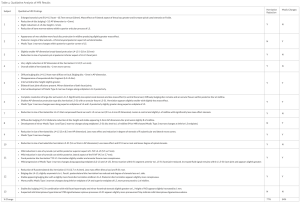
Table 1
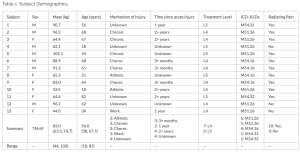
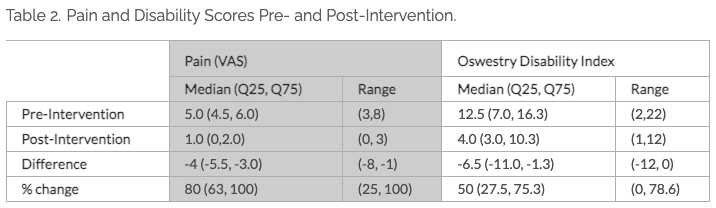
Table 2
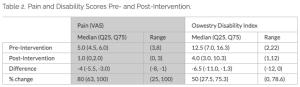
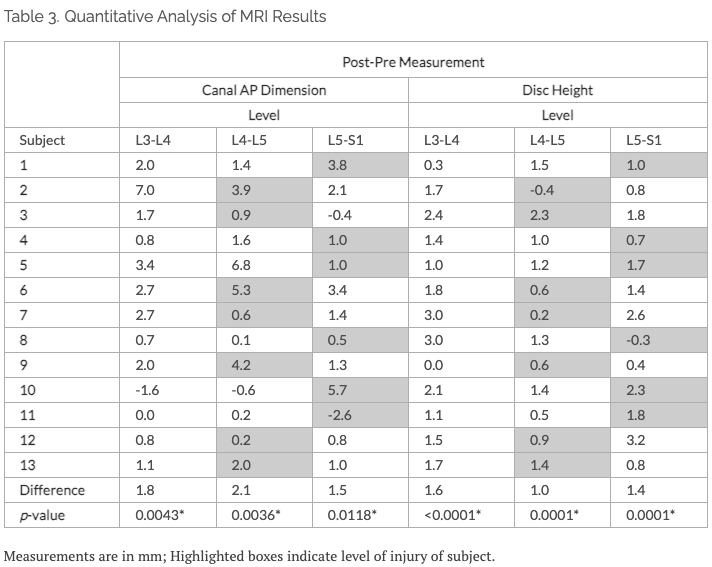
Table 3
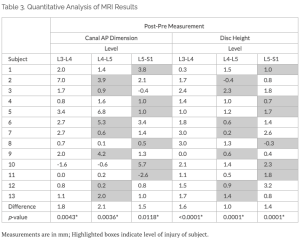
Table 4
Rosemont, IL; 2018.
Table 1
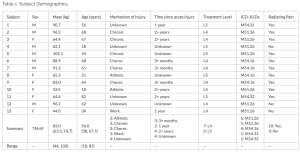
Table 2
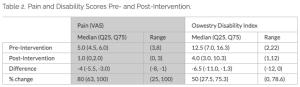
Table 3
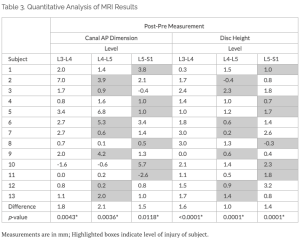
Table 4
Rosemont, IL; 2018.
Abstract
Objective:
Non-surgical spinal decompression is a conservative approach to treating lesions of the spinal column. As low back pain is a common health complaint that has a substantial economic burden laden with treatment options with poor long-term outcomes, it is requisite to explore the non-pharmacological application of non-surgical spinal decompression to treat common presentations of spinal lesions (intervertebral disc, sciatica, degenerative disc disease, etc.).
Clinical Features:
In this case series, we present 13 patients (7 male; 6 female; age 18-82 years) with a broad presentation of intervertebral disc lesions (level, radiating pain, disability, etc.). Patients were selected from a convenience sample of those that had both pre- and post-intervention MRIs. Two separate radiologists provided independent medical imaging impressions.
Intervention and Outcome:
After confirming diagnosis via MRI, these patients received 20 treatments of non-surgical spinal decompression delivered with the DRX9000. Clinical examination was performed and outcome measures of pain, disability, and subjective improvement of activities of daily living were assessed both pre- and post-intervention.
Conclusion:
The results demonstrated that there was significant (p<0.001) improvement of pain (80%), disability (50%), and subjective recovery (75%). Further, both the average disc height and canal anterior-posterior dimension increased by 1.0-1.6 mm and 1.5-2.1 mm, respectively. Thus, non-surgical spinal decompression demonstrated good to excellent clinical outcomes as a conservative, non-surgical treatment for intervertebral disc lesions.
Introduction
Low back pain (LBP) is 1 of the highest incidence of medical conditions contributing to disability, decreased activities of daily living (ADL), decreased quality of life (QoL), and inability to work (US and worldwide).1,2 LBP affects approximately 70-85% of people during their lifetime,3,4 with about 20% becoming chronic (age 20-59).3 As a leading musculoskeletal (MSK) condition, LBP largely contributes (~21%) to US financial burden (approximately $980B annually; 5.8% of US Gross Domestic Product).1,5 In fact, LBP has been the leading cause of disability for numerous decades.6 Further, many chronic MSK pain patients do not respond to surgery7–10 and many develop dependence on opioids.11,12
There is reason for alarm with current clinical approaches to treating chronic LBP. For those who visit the emergency room for LBP, 45% are prescribed opioids.13 Even outside of the emergency room, opioid prescription increases 4.7% later in the day at primary care clinical appointments.14 A recently published report (Jones et al.) of a randomized placebo-controlled trial for opioid analgesia on acute LBP found that opioids should not be recommended as there is not any measurable difference in pain severity compared with placebo after 6 weeks, and no further difference of pain at 1 year.15 Jones et al. strongly recommend a change to the frequent use of opioids for MSK conditions.15 Regarding surgery for LBP, at an average 3.4 years after surgery, the overall prevalence of failed-back surgery syndrome was 20.6%.9 Further, the residuals of these cases demonstrated 94% with LBP, 69.8% with numbness, 43.3% with cold sensations, and 35.3% with paresthesia.9 Severe LBP prior to surgery demonstrated an odds ratio of 15.2 (7.8-29.7) to develop failed-back surgery syndrome.9 Within the diagnoses monitored in this failed-back surgery syndrome study, 89.3% would be eligible for conservative approaches to treatment.9 Rates of spinal fusion surgery are highest in the US, with rates 5x that of the United Kingdom and 2x that of other developed countries (e.g., Australia, Canada, Finland, etc.).16 Failure rates for spinal surgery have remained unchanged for decades, despite spinal surgery rates increasing,17 demonstrating a knowledge gap of the mechanics of either LBP or of the prescribed clinical interventions.
Between 1990-2000, there was a 220% increase in spinal fusion surgery, despite no clear indication and absence of demonstrated efficacy.16 From these increased spinal surgeries, for those that have had one back surgery, 30% obtained adequate pain relief and up to 70% had repeat surgeries.18 Even if spinal decompressive surgeries have reduced pain, long-term degenerative changes are evident in 90% of patients, with loss of disc height (89%), facet joint arthritis (89%), endplate changes (57%), and 97% reporting pain during the last 12 months.19 Clearly, even with advances of surgical instrumentation and less invasive procedures, surgical intervention for chronic LBP may be heavily overutilized when non-invasive and more conservative approaches were not first exhausted. Surprisingly, the best results from spine surgery (regarding pain and function) occur in regions with the lowest surgical rates.20
With current ambiguities of LBP care, patients and clinicians often inadvertently circumvent non-invasive/conservative approaches that can alleviate pain and suffering and pursue costly/painful surgeries (average $22,890 ± $6,323)21 or potentially addictive pharmaceuticals that do not yield better outcomes.1 Low back surgeries can be costly and affect both immediate and long-term health due to long recovery or failed surgeries.22,23 The current treatment options for bulging, protruding, or herniated intervertebral discs (IVD), degenerative disc disease, facet syndrome, and sciatica most commonly include corticosteroid injections, non-steroidal anti-inflammatories, opioids, muscle relaxers, or surgery.24 Many of these therapeutics have detrimental long-term effects, undesired side effects, are invasive procedures with low success rates, and further, do not fare better than conservative care after 6 months.13 Clearly with the widespread incidence of LBP and its effects on activities of daily living (ADLs) and quality of life (QoL), there is a need for innovative therapeutic approaches that better address the burden of difficult spinal disease. Aside from the success of manipulative therapy for LBP,5,25–27 more severe LBP originating from damaged or degenerative IVDs, facet syndrome, or sciatica may require additional interventions such as non-surgical spinal decompression (NSSD).28 In fact, even though spinal manipulations (e.g., chiropractic) have demonstrated evidence of successful alleviation of LBP,29–31 many practitioners still do not know how to or whether to treat a herniated disc and spinal manipulation may not be the ideal treatment.32
With the widespread incidence of LBP and its effects on ADLs and QoL, there is a need for innovative therapeutic approaches, such as NSSD,28 that better address the burden of difficult and chronic spinal disease that originates from damaged or degenerative IVDs, facet syndrome, or sciatica. The DRX9000 is a mechanical NSSD device that is in clinical use throughout the world. This device allows for axial decompression of the lumbar spine. The purpose of this case series report was to provide a diverse evaluation of multiple patients with their presentation and outcomes from their course of treatment on the DRX9000.
Methods
This study followed all ethical guidelines for retrospective record review with oversight of the University of South Florida Internal Review Board (STUDY004354). The University of South Florida Chiropractic Clinic began treating patients on the DRX9000 in December 2023. From the patients treated to date, we selected a convenience sample of 13 cases (Table 1) selected from those that had both pre- and post-MRI imaging of the lumbar spine and performed on the same MRI coil for both time points to minimize variance. The patients presented with various forms of other prior treatments for their LBP, including activity modification (54%), chiropractic (54%), physical therapy (69%), interferential current (54%), non-steroidal anti-inflammatory (77%), steroid (15%), muscle relaxer (8%), spinal injection (23%), and spine surgery (8%). The individual with prior spine surgery which was a laminectomy/discectomy L4/L5.
Clinical examination included straight leg raise (23% positive), toe walk test (23% positive), heel walk test (23% positive), slump test (38% positive), Faber test (8% positive), Fortin Finger test (8% positive), Kemp test (31% positive), Patellar reflex (85% evaluated), and Achilles reflex (85% evaluated). In addition, each patient had an MRI scan of the lumbar spine prior to treatment to verify their diagnosis.
Two radiologists (WRM, neuroradiologist; ST, Diplomate of the American Chiropractic Board of Radiology) independently reviewed both pre- and post-intervention MRIs for each subject. Both radiologists were requested to read the MRIs as typical for their standard of care. WRM performed measurements of spinal canal anterior-posterior (AP) dimension and disc height for all levels T12-S1, however as the levels treated for this cohort were either L4 or L5, only levels L3-S1 were reported. AP diameter was measured from the herniation to the posterior wall of the canal. ST provided radiology reports which included both qualitative and quantitative results.

Results
Each of the 13 patients received 20 sessions of NSSD of the lumbar spine at the respective level of their diagnosis. The treatment ranged from 2-3 times per week, with more aggressive frequency at treatment initiation. The median treatment time was 1412,15 weeks. The minimum tension of the decompression was 36.7 (27.0, 42.2) kg (38.0–45.7% body mass); the maximum tension was 45.8 (36.1, 51.3) kg (54.2–59.8% body mass).
All 13 patients have received a post-intervention MRI on the same coil as their pre-intervention MRI. To date, the 13 patients have a median follow-up time of 96,12 months. Only 1 of the 13 patients had a recurrence of pain after 8 months in which they underwent 11 additional treatments to return to prior pain and functional status. Pain and disability scores from patient reported outcomes are summarized in Table 2. Overall, patients had a median pain decrease of -4 (-5.5, -3.0), which was an 80% improvement. A paired t-test demonstrated a difference in pain score pre- to post-intervention (t7=-7.283; p<0.001). Further, the patients had a decrease of -6.5 (-10.6, -1.9) on the Oswestry Disability Index that similarly was different when evaluated by a paired t-test (t7=-3.416; p=0.011), a 50% improvement. Subjectively, at termination of treatment, patients stated that they had an overall improvement of their function and activities of daily living by 75% (70, 86.2) with an overall range of 40-98%.
MRI analyses are summarized in Table 3 and Table 4. The AP Dimension increased 1.5-2.1 mm (p≤0.0118). Disc height increased 1.4-1.6 mm (p≤0.0001). Further, from a qualitative assessment of the MRIs, we determined a quantitative reduction of disc herniation of 77% and Modic changes (Type I and Type II) for 54% (Table 4).
DISCUSSION
This case series demonstrated successful outcomes of pain, disability, medical imaging, and subjective scale of improvement across a diverse population. The patients were represented from a broad age range (18-82 years), both sexes, varying mechanisms of injury, and a diverse timeframe after injury, allowing for the results to be generalized to a broad population. Overall, the patients demonstrated ‘good’ to ‘excellent’ clinical results of NSSD with the use of the DRX9000. Pain decreased significantly after 20 NSSD treatments with an improvement of 80%. Disability similarly improved by 50%. Further, patients subjectively reported that their overall symptoms and activities of daily living improved by 75%. In addition, objective MRI measurements demonstrated significant increases of both disc height and AP dimension.
The timeframe after the acute injury of the patients is important in this report as there is evidence that IVD injury can spontaneously heal within the acute timeframe (3-6 months) due to inflammatory pathways and macrophage activation.33–35 In this cohort of patients, half had a timeframe of a IVD lesion greater than 12 months and 3 of 4 that were ‘unknown’ were classified as such due to either a chronic IVD lesion (n=1) or an unknown mechanism of injury (n=2), likely making these chronic cases. Chiu et al. performed a meta-analysis of 9 peer-reviewed articles from 1992-2006 that included lumbar herniated IVDs not treated with surgical intervention.36 The selection criteria required that an individual study include at least 2 images (myelography, CT, or MRI), taken at baseline and follow-up, as their method of investigating disc regression. The results of their study (n=361 IVDs) demonstrated that the IVD lesion severity is largely related to the degree of spontaneous IVD lesion regression.36 Specifically, spontaneous resolution was 11.1% for bulges, 0% for protrusions, 15.0% for extrusions, and 42.9% for sequestration. Most disc regression happens within the first year, with observable regression within 237 or 3 months.38 In this case series, all 13 subjects had lumbar lesions of a chronic nature that had not spontaneously resolved. However, after 20 treatments of NSSD, 77% had notable changes of a herniated disc, including disappearance of a sequestered disc fragment (Subject 5). Interestingly, 54% demonstrated Modic changes at the vertebral endplates, which may be an indicator of a healing inflammatory process due to biomechanical forces in the absence of pain.39 Spontaneous regression of herniated lumbar IVDs may be due to some type of mechanical NSSD that the patient received, whether through activities of daily living or other forms of decompression. Further, it is possible that mechanical traction/stretching induces macrophage activation and an immune response40 to a region of the body that is considered to be immune privileged.41 Consequently, with the protection of the IVD from macrophage activity, it is possible that NSSD provides faster resolution of the IVD by 1) creating a negative pressure within the IVD resulting in increased disc height42,43 and 2) by complementing the inflammation pathway to allow for remodeling of the herniation, bulge, or sequestration with macrophage activity.33–35,40
This case series is limited by both absence of subject blinding and randomization to treatment group. Further, post-intervention examination could have been performed to report improved objective outcomes from the intervention (e.g., heel walk, toe walk, straight leg raise, etc.) and should be performed for future studies. The 13 patients included were not hand-selected as the ‘best cases’ from the eligible lumbar spine cases from the USF chiropractic clinic. Rather, cases were selected based on those that had both pre- and post-intervention MRI imaging on the same MRI coil to minimize potential image interpretation bias due to data acquisition parameters. Although this selection procedure was not random, the convenience sample negated investigator selection bias for the 13 cases included.
CONCLUSION
The results presented demonstrated that DRX9000 NSSD is a viable, conservative option for treating lumbar lesions of the IVD with a high value for both subjective and objective clinical results. Although this report is not a cohort or randomized clinical trial, the high quantity of patients included in the case series and the broad generalizability of the population provides substantial evidence to support the use of NSSD for treatment of lumbar IVD lesions. Further, it provides foundational support to pursue additional clinical research on its effectiveness and longevity of positive results.
LEARNING POINTS
- Non-surgical spinal decompression produced significant improvements of pain and disability.
- Patients reported a positive subjective recovery (75%) for their condition and activities of daily living.
- Objective MRI measurements demonstrated increased disc height and AP dimension
Acknowledgements
We acknowledge financial support from the Florida Department of State Center for Neuromusculoskeletal Research, the Florida High Tech Corridor (FHD-24-014), and Excite Medical. We would like to acknowledge the assistance of Anaiz Elizondo in coordination of MRI reads with author WRM.
Conflicts of Interest
All authors maintain full academic freedom to publish all results, whether positive or negative, related to funding provided in part by Excite Medical.
Submitted: February 20, 2025 CDT Accepted: March 03, 2025 CDT