Retrospective Chart Review of Nonsurgical Spinal Decompression as a Therapeutic Modality for Low Back Pain
Military Medicine, Volume 190, Issue Supplement_2, September/October 2025, Pages 134-140 | Published: 16 September 2025
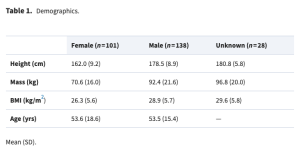
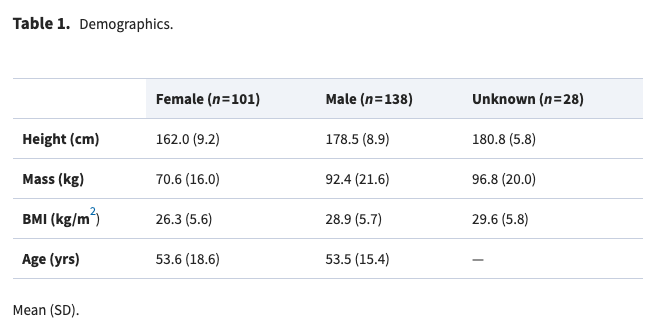
Table 1
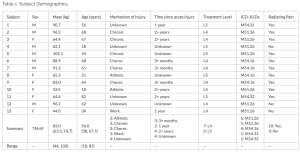
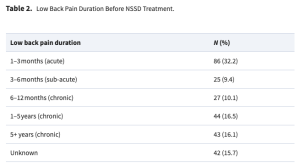
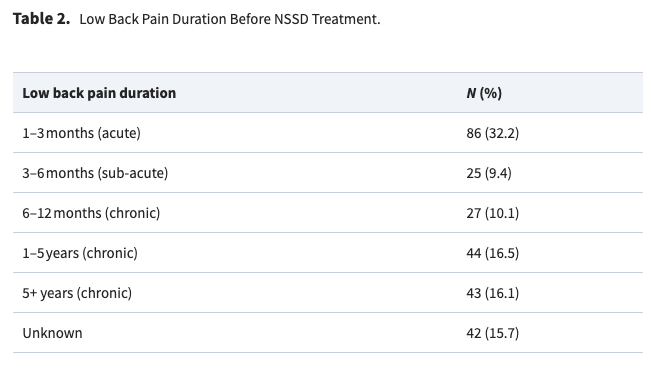
Table 2
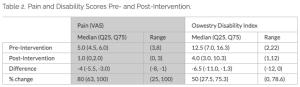
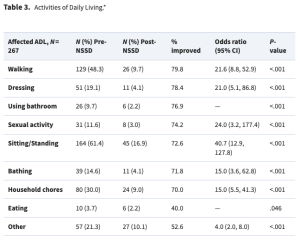
Table 3
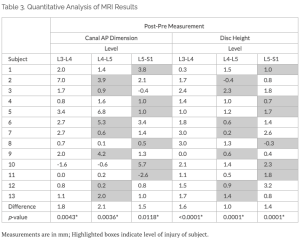
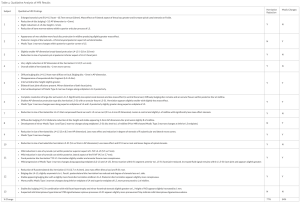
Table 4
Rosemont, IL; 2018.
Largest non-surgical spinal decompression study in nearly three decades published by Oxford University Press in the International Journal of AMSUS (Military Medicine).
Please see the full study here.
Abstract
Introduction:
Low back pain (LBP) is a leading cause of disability and health care costs worldwide. Despite its prevalence, many patients fail to respond to surgical interventions and often face opioid dependency. Nonsurgical spinal decompression (NSSD) is a conservative treatment that may alleviate LBP by decompressing intervertebral discs, but it remains underutilized as a result of limited evidence and lack of insurance coverage.
Methods:
This retrospective chart review aimed to evaluate the effectiveness of NSSD and LBP outcomes, including pain intensity, neurological function, and activities of daily living (ADLs) from community clinics nationwide. A total of 267 patient records from 7 clinics were analyzed. Patients underwent ≥20 NSSD sessions for over 6 to 8 weeks, with a median of 2 treatments per week. Demographics, subjective pain scores, clinical examination (reflex, myotome, and dermatome tests), and ADLs were collected. Statistical analyses included McNemar’s, matched pairs t-tests, and subgroup analyses using a Kruskal-Wallis test of duration of current LBP.
Results:
The cohort demonstrated significant improvements in all measured outcomes. Pain scores were decreased by an average of 4.4 points (from 6.9 to 2.5; P < .001), with 90.5% of patients reporting pain reduction. Reflexes, myotomes, and dermatomes showed improvements of 60.9%, 74.8%, and 77.6%, respectively. ADLs improved significantly, with odds ratios ranging from 4.0 to 40.7 (P < .001). Subgroup analyses revealed consistent benefits across different chronicity levels of LBP.
Conclusion:
These findings suggest NSSD is an effective conservative treatment for a diverse population with LBP, addressing pain, neurological deficits, and functional impairments. NSSD may offer a cost-effective alternative to surgical interventions and pharmacological treatments, reducing the risks of opioid dependency and surgical complications. Future studies should include randomized controlled trials and long-term follow-ups to further validate these results. This study emphasizes NSSD as a first-line therapy for LBP, warranting broader adoption and coverage to improve patient outcomes and reduce health care costs.
Introduction
Low back pain (LBP) is one of the most prevalent spinal conditions worldwide, impacting millions and contributing a considerable portion of health care expenses and productivity losses, with annual U.S. financial burden at approximately $980B annually (5.8% of the Gross Domestic Product).1,2 LBP accounts for one of the highest incidence medical conditions that contributes to disability, decreased activities of daily living (ADL), decreased quality of life, and inability to work (United States and worldwide).1,3 In fact, of all diseases and injuries that contribute to disability-adjusted life years in the United States, LBP ranks third.4 LBP affects approximately 70 to 85% of people during their lifetime,5,6 with approximately 20% becoming chronic (age 20-59 years).5 LBP has been the leading cause of disability for numerous decades.7 Furthermore, many chronic musculoskeletal pain patients, especially with LBP, do not respond to surgery8 and many develop dependence on opioids.9
As a result of the physical demands of military service, Armed Forces personnel often bear the brunt of chronic pain conditions.10 Veterans are more likely to have LBP (32.8%) and experience pain at younger ages compared to nonveterans.10 LBP among active duty Soldiers is 40.5 per 1,000 person-years,6 a rate 2× higher than the civilian population.10 This number is likely underreported as active duty Soldiers may not report injuries for fear that the injury might affect future career opportunities and mandated physical restrictions.11 Musculoskeletal conditions and injuries are the leading cause of chronic pain and painful musculoskeletal conditions are the leading cause of limited duty days, inability to deploy, and disability.12,13 Thus, efficaciously treating chronic LBP is of high importance for the U.S. military.
There is reason for alarm with current clinical approaches to treating chronic LBP, especially for the U.S. military. For those that go to the emergency room for LBP, 45% are prescribed opioids.14 Similarly, steroid injection has largely been shown to not be effective in treating intervertebral disc (IVD) lesions.15 Heavy reliance on opioids or other pain medications can impair military operational decisions and carry risks of dependency. Spinal surgeries, particularly fusion procedures, are associated with significant health care costs.16,17 These procedures have recently come under scrutiny for likely overuse, demonstrating less improvement than expected, and disproportionately expensive compared to the potential benefit.16,18 Consequently, many medical experts advise against spinal surgery when LBP can be successfully managed conservatively.19
Nonsurgical axial spinal decompression (NSSD) is a conservative and noninvasive treatment that can counteract the effects of gravity to decompress the spine to alleviate IVD lesions.20,21 Currently, there is limited scientific evidence that currently supports NSSD as an effective treatment for back pain, NSSD is not reimbursed by health insurance. In addition, NSSD devices have not been adequately studied as conservative treatment alternatives to back surgery. Thus, the purpose of this retrospective chart review was to evaluate the outcomes of NSSD for the treatment of LBP and its generalizability. We hypothesized that NSSD would demonstrate improvement of LBP specifically with activities of daily living, neurological reflexes, myotomes, dermatomes, and diminished pain intensity.
Methods
This study was reviewed and approved by the University of South Florida Institutional Review Board (STUDY004354). This retrospective chart review was designed to collect demographic, clinical presentation, treatment parameters, and patient-/clinician-reported outcomes from chart notes relating to patients receiving NSSD for LBP by a certified health care professional.
This study was partially sponsored by Excite Medical (Tampa, FL), the manufacturer of NSSD devices (DRX9000®). A list of clinics with NSSD devices was compiled from the company and a REDCap survey was e-mailed to these clinics to solicit willingness to participate in contributing data to the retrospective chart review. Of the original 899 clinics, 24 (2.7%) expressed an interest in providing data for the study. In addition to the e-mail survey, the study was communicated during national continuing education presentations (n = 3) to clinical providers of NSSD (i.e., osteopaths, chiropractic, medical doctors). Clinics verified to submit data (n = 9) were provided an encrypted server on which to upload de-identified data. These data were then entered manually onto a REDCap server for data storage and integrity. After data entry of the records into REDCap and confirmation of data integrity, the de-identified records provided by the clinics were deleted from the original encrypted server.
Patient records were accepted over a 16-month period from March 2023 to July 2024. Inclusion criteria were patients aged 18+ years who had undergone NSSD for the lumbar spine for at least one session. Practices were encouraged to submit all their available cases regardless of whether there were successful NSSD treatment outcomes to allow for improved generalizability. Pertinent data included clinic type, health care provider type, patient demographics, clinical observations, treatment parameters, and subjective- and objective-reported outcomes. With visual pain scaling, scores were reported between 0 (no pain) and 10 (excruciating pain). Clinical observations of interest included neurological examination of deep tendon reflexes (i.e., patellar, achilles), muscle strength examination (myotomes), and dermatomes (sensation).
NSSD treatment is performed with a patient lying in the supine position after the patient is fitted with a harness. A cable from the NSSD machine attaches to the inferior end of the harness, and the cable angle is adjusted to specific angles based on patient height and specific vertebral segment targeted. Force is set based on the patient’s mass. As this was a retrospective chart review, no standardized methods for treatment parameters, clinical observations, ADL reporting, and reported outcomes were used. All variables were recorded from documentation in clinical “SOAP” notes. The method of collection by individual clinics was not annotated and is therefore unknown.
JMP Pro 17 (SAS; Cary, NC, USA) statistical software was utilized to perform all statistical analysis. Distributions were utilized to assess all demographic, treatment characteristics, pain, ADL, reflex, myotome, and dermatome outcomes. Demographics were separated for males and females so that generalizability of the data can be interpreted by sex. McNemar’s test was used to evaluate paired pre- to postchanges in reflex, myotome, and dermatome findings, as well as changes to ADLs as a result of the NSSD intervention. Each of these variables was dichotomous—either “present” or “absent”—based on either the examination or ADLs reported by the patient. From McNemar’s test, odds ratios were calculated from the ratio of those that improved from the treatment over those that got worse from the treatment. A matched pair t-test, comparing individual changes in pain pre- to post-treatment was used for pain measures. In a sub-group analysis, Kruskal-Wallis was used to determine whether pain differences were higher according to duration of current back pain. An alpha level of <0.05 was set for significance a priori.
Results
Patient demographics (n = 267) are summarized in Table 1. Patients were distributed between sexes (101 F:138 M) with an average age of 53.3 ± 16.7 years. Although height, mass, and body mass index (BMI) were significantly different between sex groups, subgroup analyses of sex were not performed for the selected outcome variables. Race was not well reported, with unknown values more prevalent than known (Asian = 3; Black = 3; White = 76; Mixed = 1; Unknown = 184). Demographic records were from a variety of medical practice types (Group practice = 54; Hospital = 42; Private clinic = 171) with 21.5% referred to other interdisciplinary treatment. Of the 267 subjects, 19 (7.1%) were referred for NSSD treatment from a spine surgeon. In addition, 15 (5.6%) had reported a prior spine surgery. Diagnoses included lumbar IVD lesion (n = 111; 41.6%), lumbar IVD with radiculopathy/myelopathy (n = 48; 18%), sciatica (n = 22; 8.2%), unspecified or generalized low back pain (n = 13; 4.9%), lumbar spondylosis (n = 10; 3.7%), postlaminectomy syndrome (n = 3; 1.1%), lumbar spinal stenosis (n = 2; 1%), and unknown (n = 58; 21.7%). The primary diagnosis location was dispersed across the lumbar spine with L4-L5 IVD being the most common lesion (Supplementary Table 1). The duration of LBP ranged from acute to chronic (Table 2).
Nonsurgical Spinal Decompression Treatment
Among all subjects, NSSD was performed for a median of 28 [28, 30] min, with an average load of 365.5 ± 141.5 N. The treatment duration was ≥8 weeks for 67%, 6 to 8 weeks for 22%, and <6 weeks for 11% of participants. It was unclear based on charting methods whether this shorter duration was prescribed or occurred as a result of patient drop-out. The median treatments per week were 2 [2, 3] with a range from 1 to 5. The total quantity of treatments was 20 [20, 25] with a range from 1 to 97.
Pain
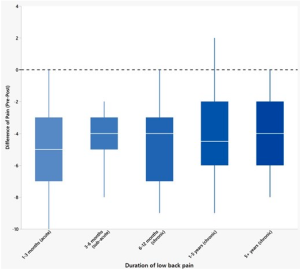
Among the patients with standard-of-care visual pain scaling (n = 220), the median initial pain level on a scale from 0 to 10 was reported as 7 [6, 8]. From NSSD treatment, pain decreased to 4.4 (−4.0, −4.7) points. Only 1% (n = 2) reported an increase of pain (2.5 [2, 3]), and 7.1% (n = 19) reported no change in pain. Of those with a pain decrease, the percentage decrease of pain was 70 [50, 86]%. A matched pair t-test demonstrated an overall initial pain value of 6.9 that decreased 4.4 points to 2.5 (P < .001). A Kruskal-Wallis analysis of pain improvement by LBP chronicity demonstrated no significant differences between LBP chronicity groups (Figure 1, P = .389).
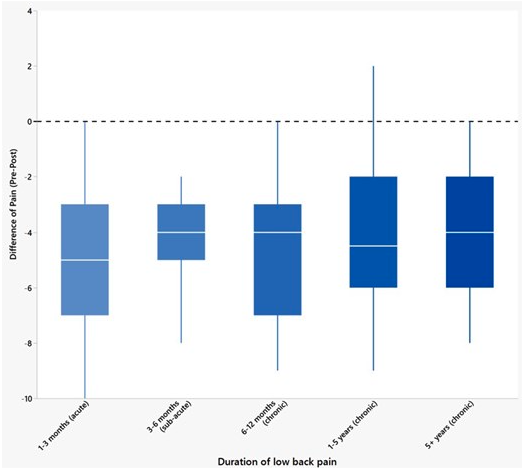
Difference of pain by LBP chronicity. Pain decrease between the various phases of LBP chronicity was not different between any of the groups. Negative values show a decrease in pain with treatment, where 0 is no change in pain pre- to post-treatment.
Activities of Daily Living
All ADLs showed improvement following NSSD treatment (Table 3). Sitting/standing and walking were the most reported ADLs to be affected by LBP. Sitting/standing and sexual activity had the largest odds for improvement following NSSD treatment.
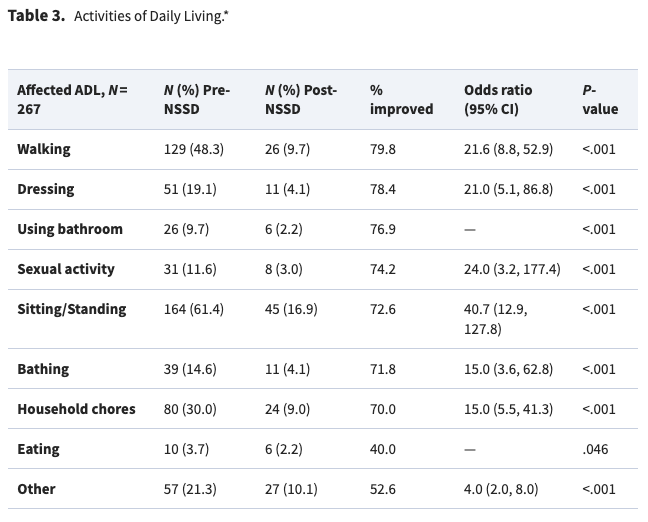
Affected activities of daily living (ADL) as annotated within clinical “SOAP” notes. *Denotes statistically significant odds ratio. Empty cells denote calculations that are “undefined” (divided by zero).
Reflexes
Of the patients observed, reflex examination was documented in 203 out of 267 (76%) patients at their initial visit (L4 = 62; L5 = 47; S1 = 66; Other = 3; Unknown = 25). There were 92 patients with reflexes affected (absent, hypoactive, or hyperactive) before, and 36 with reflexes affected after treatment (overall improvement 60.9%). When all reflexes were combined for analysis (L4-S1), they had odds of 57.0 (7.9, 411.6) to improve with NSSD treatment (P < .001). As neurological examination is considered a part of standard practices, it is unclear if the remaining 24% of patient did not have a neurological examination performed, or the provider failed to document it accordingly.
Myotomes/Dermatomes
Only 156 charts (58.4%) reported examination of myotomes (T12-S1), and 142 (53.2%) reported examination of dermatomes (L1-S1) at initial visit. There were 103 patients with myotomes affected (muscle weakness) before, with 77 (74.8%) reporting improvement after treatment. Myotomes, when combined for analysis, had odds of 78.0 (10.9, 560.7) to improve with NSSD treatment (P < .001). There were 76 patients with dermatomes affected (decreased sensation) before treatment, with 59 (77.6%) reporting improvement after treatment. Dermatomes had odds of 20.7 (6.5, 65.8) to improve with NSSD treatment (P < .001).
DISCUSSION
The results of this retrospective study demonstrate a robust effect of NSSD for treatment of LBP conditions. Specifically, there was a remarkable improvement in all tracked ADLs, with odds ratios of improvement ranging from 4.0 (Other) to 40.7 (Sitting/Standing; Table 3). Furthermore, there was a remarkable improvement of L4-S1 reflexes with odds at 57.0. Affected myotomes had odds of 78.0 to improve; affected dermatomes had odds of 20.7 to improve. Finally, subjective pain reports improved by −4.4 points on visual pain scaling. Pain decreased the same for each classification of LBP pain chronicity (Figure 1). Taken together, this demonstrates that a diverse set of low back pain patients—by diagnosis, chronicity of condition, sex, and age—experienced improvement of NSSD treatment on ADLs, subjective pain, and altered reflexes, myotomes, and dermatomes with a median of 20 NSSD treatment sessions. Our hypothesis that NSSD would demonstrate improvement of LBP for ADL, neurological reflexes, myotomes, dermatomes, and diminished pain intensity was supported. Thus, for those who’s ADLs are affected by LBP, NSSD may offer a conservative approach to treatment as it demonstrated a high odds for improvement across various ADL outcomes compared to those who did not have affected ADLs.
Compared to prior retrospective research with mechanical NSSD (not manual or autotraction), the initial pain on a 0 to 10 scale of our cohort (6.9) was similar to that previously reported at 6.1 and 6.3.22,23 Similarly, the reduction of pain of our cohort (−4.4) was similar to that previously reported (−4.6 and −5.2).22,23 These prior retrospective analyses of NSSD reported outcomes on 30 and 94 patients.22,23 This current analysis, with a similar approach, has increased the analysis by nearly 3- to 10-fold and provides further substantiative evidence of the various treatment outcomes of NSSD.
When faced with debilitating LBP, especially chronic LBP, a patient will seek solutions that allow them to return to normal activities with minimal pain.1 With current ambiguities and no clear systematic approach to LBP care,18 many LBP patients may inadvertently circumvent noninvasive or conservative therapeutic approaches that can alleviate pain—such as NSSD—at a fraction of the cost of other approaches (likely 10-20%). Furthermore, conservative intervention as a first approach to LBP treatment may help avoid costly surgeries (average cost $22,890 ± $6,32324; up to $110,00016) or potentially addictive pharmaceuticals that may not yield better outcomes.1
Current first-line treatment options for bulging, protruding, or herniated IVDs, degenerative disc disease, posterior facet syndrome, and sciatica most commonly include corticosteroid injections, nonsteroidal anti-inflammatories, opioids, and muscle relaxers.25 A recently published report of a randomized placebo-controlled trial for opioid analgesia on acute LBP found that opioids should not be recommended as there is no difference in pain severity compared with placebo after 6 weeks, and no further difference of pain at 1 year.26 Jones et al. strongly recommend a change to the frequent use of opioids for musculoskeletal conditions.26 Pharmacotherapeutics, although effective at diminishing pain in the short term, may have detrimental long-term effects, undesired side effects, and do not fare better than conservative care after 6 months.14
Although NSSD may not be the correct solution for all patients, they should be aware of LBP treatment options and their reported outcomes. Regarding LBP surgery, at an average 3.4 years after surgery, the overall prevalence of failed-back surgery syndrome is 20.6%.8 Furthermore, the sequelae of these failed cases demonstrate 94% with LBP, 69.8% with numbness, 43.3% with cold sensations, and 35.3% with paresthsia.8 Severe LBP before surgery demonstrates odds ratio of 15.2 (7.8-29.7) to developing failed-back surgery syndrome.8 Alarmingly, rates of spinal fusion surgery across the globe are highest in the United States, with rates 5× that of the United Kingdom and 2× that of other developed countries (e.g., Australia, Canada, and Finland).27 Failure rates for spinal surgery have remained unchanged for decades, despite spinal surgery rates increasing.28 Between 1990 and 2000, there was a 220% increase in spinal fusion surgery, despite no clear indication and absence of demonstrated efficacy.27 From these increased spinal surgeries—for those that have had one back surgery—only 30% obtained adequate pain relief and up to 70% had repeat surgeries.29 Even if spinal decompressive surgeries (some with fusions) have reduced pain, long-term degenerative changes are evident in 90% of patients, with loss of disc height (89%), facet joint arthritis (89%), adjacent segment modic-type changes (83%), endplate changes (57%), and 97% reporting pain during the last 12 months.30 Clearly, even with advances of surgical instrumentation and the introduction of minimally invasive procedures, surgical intervention for chronic LBP may be heavily overutilized when noninvasive and more conservative approaches were not first utilized. Surprisingly, the best results from spine surgery (with regard to pain and function) occur in geographical regions with the lowest surgical rates.31
With the widespread incidence of LBP and its effects on ADLs and quality of life, there is a need for therapeutic approaches that better address the burden of difficult spinal disease. Aside from the successes that manipulative therapies (e.g., chiropractic, osteopathy) and physical therapy have demonstrated for alleviation of LBP,32,33 more severe LBP that originates from damaged or degenerative IVDs, facet syndrome, or sciatica may require additional interventions such as NSSD.34 In fact, many practitioners may not know how or whether to treat a herniated disc; and spinal manipulation may not be the ideal treatment.
With respect to active duty Soldiers or Veterans, they face the brunt of chronic pain conditions at a rate twice that of the civilian population.10 Veterans are more likely to have LBP (32.8%) and experience pain at younger ages compared to nonveterans.10 Thus, the results of this study are pertinent to the military as the outcomes for LBP pain reduction, improved neurological function, and return of ADLs would be vital to ensuring military readiness. Further, these results are available for LBP at a fraction of the cost for low back surgeries, which can affect both immediate and long-term U.S. military health and readiness because of long recovery or failed surgeries.13,35 Although the average age for this study is higher than most active duty Soldiers, the average BMI is similar to that of active duty service members,36 and the data is valid for Veterans. As Veterans and active duty Soldiers often have comorbidities with chronic LBP (e.g., traumatic brain injury, post-traumatic stress disorder, depression, anxiety, substance use disorder, and sleep disorders),13 these comorbidities can complicate both patients’ experiences of chronic pain and providers’ approaches to treatment.13 Thus, there is need for further research of NSSD with these comorbidities being explored and documented.
This study could be subject to selection bias, as there is the possibility that only those cases that were the most successful were transmitted to the investigators and included in the study. However, our results strongly resemble those of other published studies.22,23 Another limitation is that there was no control group, making it difficult to determine if the benefit of NSSD could be because of a placebo effect. However, provided that the majority of patients included had chronic LBP (≥6 months), this effect is unlikely as most patients would have attempted numerous therapeutics prior. In addition to NSSD, some of the patients may have received other concomitant modalities (e.g., spinal manipulation, electrical stimulation, heat, ice, physical therapy), thus the results may not directly demonstrate solely the therapeutic effect of NSSD. Additionally, analyses were not adjusted for confounding variables such as age, sex, or comorbidity status, which may have further effect on these results. To further establish evidence for NSSD, future work could include a follow-up survey to the included 267 patients to determine their long-term success of NSSD treatment as well as further subgroup analyses of sex differences as a result of group differences in height and mass, which are important factors in NSSD treatment. In addition, more randomized clinical trials should be conducted with NSSD.
CONCLUSION
This study demonstrates a robust effect of NSSD with administration of a median of 20 NSSD treatments on LBP and quality of life. There were high odds of improvement with both objective and subjective outcomes; specifically, there was improvement among those affected across all ADLs (40-79.8%), reflexes (60.9%), myotomes (74.8%), dermatomes (77.6%), and reduction of pain (90.5%). These rates for the conservative treatment of common LBP diagnoses (lumbar IVD lesions, radiculopathy, myelopathy, spondylosis, and sciatica), demonstrate convincing evidence for utilizing NSSD as a first-line treatment approach before consideration of other long-term therapeutics such as injections, discectomies, and fusions.
ACKNOWLEDGMENTS
The authors would like to acknowledge the following clinical practices for providing de-identified patient records for inclusion in this research study: Advanced Rehabilitation & Medical, Advanced Spine & Sports Care, Cary Disc Center, Deland Chiropractic, Hospital San Angel Inn Universidad, Life University, Spine & Sport Rehabilitation Institute, Wakeman Chiropractic, and Well Health & Chiropractic.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Military Medicine online.
FUNDING
The authors acknowledge funding from the Florida High-Tech Corridor (FHT 23-01) in partnership with Excite Medical (N.D.S.). Additional funding was provided by the National Board of Chiropractic Examiners (S.S.) and the Florida Department of State Center for Neuromusculoskeletal Research (N.D.S.).
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
The data from this study are available upon reasonable request to the corresponding author.
INSTITUTIONAL REVIEW BOARD APPROVAL
University of South Florida, STUDY004354
INDIVIDUAL AUTHOR CONTRIBUTION STATEMENT
The authors confirm contribution to the manuscript as follows: Study conception and design (N.D.S.); Data collection (S.S., G.A.M., N.D.S.); Analysis and interpretation of results (S.S., L.L., G.A.M., N.D.S.); draft manuscript preparation (S.S., N.D.S.). All authors reviewed the results and approved the final version of the manuscript.
INSTITUTIONAL CLEARANCE
Not applicable.
References
See here.